Abstract
Background
“Textbook oncologic outcome” (TOO) is a composite quality measure representing the “ideal” outcome for patients undergoing cancer surgery. This study sought to assess the validity of TOO as a metric to evaluate hospital quality.
Methods
Patients who underwent curative-intent resection of gastric, pancreatic, colon, rectal, lung, esophageal, bladder, or ovarian cancer were identified in the National Cancer Database (2006–2017). Cancer site-specific TOO was defined as adequate lymph node yield, R0 resection, non-length-of-stay outlier, no hospital readmission, and receipt of guideline-concordant chemotherapy and/or radiation. Mixed-effects analyses estimated the adjusted TOO rate for each hospital stratified by cancer site. The association between hospital adjusted TOO rates and 5-year overall survival was assessed using mixed-effects Cox proportional hazards analyses.
Results
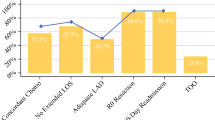
Among 852,988 cancer resections, the TOO rate varied across cancer sites as follows: stomach (31.8%), pancreas (25%), colon (66.9%), rectum (33.6%), lung (35.1%), esophagus (31.2%), bladder (43%), and ovary (44.7%). After characterization of adjusted hospital TOO rates into quintiles, an incremental improvement in overall survival was observed, with higher adjusted TOO rates. Similarly, with the adjusted hospital TOO rate treated as a continuous variable, there was a significant 4% to 12% improvement in overall survival for every 10% increase in the adjusted hospital TOO rate for gastric (hazard ratio [HR], 0.88; 95% confidence interval [CI], 0.85–0.91), pancreatic (HR, 0.90; 95% CI, 0.88–0.93), colon (0.93; 95% CI, 0.91–0.94), rectal (HR, 0.90; 95% CI, 0.87–0.93), lung (HR, 0.96; 95% CI, 0.95–0.97), esophageal (HR, 0.93; 95% CI, 0.90–0.95), bladder (HR, 0.94; 95% CI, 0.91–0.97), and ovarian (HR, 0.96; 95% CI, 0.94–0.98) cancer.
Conclusions
A direct association exists between adjusted hospital TOO rates and survival after high-risk cancer procedures. As a valid hospital metric, TOO can be used to compare the overall quality of cancer care across hospitals.

Similar content being viewed by others
References
Parina RP, Chang DC, Rose JA, Talamini MA. Is a low readmission rate indicative of a good hospital? J Am Coll Surg. 2015;220:169–76.
Merath K, Chen Q, Bagante F, et al. Textbook outcomes among medicare patients undergoing hepatopancreatic surgery. Ann Surg. 2020;271:1116–23.
Hyder O, Dodson RM, Nathan H, et al. Influence of patient, physician, and hospital factors on 30-day readmission following pancreatoduodenectomy in the United States. JAMA Surg. 2013;148:1095–102.
Sheetz KH, Dimick JB, Ghaferi AA. Impact of hospital characteristics on failure to rescue following major surgery. Ann Surg. 2016;263:692–7.
Schootman M, Lian M, Pruitt SL, et al. Hospital and geographic variability in two colorectal cancer surgery outcomes: complications and mortality after complications. Ann Surg Oncol. 2014;21:2659–66.
Kolfschoten NE, Kievit J, Gooiker GA, et al. Focusing on desired outcomes of care after colon cancer resections; hospital variations in “textbook outcome.” Eur J Surg Oncol. 2013;39:156–63.
Kulshrestha S, Bunn C, Patel PM, et al. Textbook oncologic outcome is associated with increased overall survival after esophagectomy. Surgery. 2020;168:953–61.
Standards for Oncology Registry Entry. 2021. Retrieved 10 March 2021 at https://www.facs.org/-/media/files/quality-programs/cancer/ncdb/store_manual_2021.ashx.
Measures, Reports & Tools, 2021. Retrieved 10 March 2021 at https://www.qualityforum.org/Measures_Reports_Tools.aspx.
CoC Quality of Care Measures, 2020. Retrieved 10 March 2021 at https://www.facs.org/quality-programs/cancer/ncdb/qualitymeasurescocweb.
Edge SB, Page DL, Fleming ID, et al. AJCC Cancer Staging Manual. 7th edn. New York: American Joint Committee on Cancer. Springer; 2010.
Amin MB, Byrd DR, Compton CC, et al. AJCC Cancer Staging Manual. 8th ed. American Joint Committee on Cancer. Springer, Chicago IL; 2017.
NCCN Clinical Practice Guidelines in Oncology, 2021. Retrieved 10 March 2021 at https://www.nccn.org/professionals/physician_gls/default.aspx.
Singh GK, Williams SD, Siahpush M, Mulhollen A. Socioeconomic, rural-urban, and racial inequalities in US cancer mortality: part I–all cancers and lung cancer and part II–colorectal, prostate, breast, and cervical cancers. J Cancer Epidemiol. 2011;2011:107497.
Onega T, Duell EJ, Shi X, Wang D, Demidenko E, Goodman D. Geographic access to cancer care in the U.S. Cancer Am Cancer Soc. 2008;112:909–18.
Xu Z, Becerra AZ, Aquina CT, et al. Emergent colectomy is independently associated with decreased long-term overall survival in colon cancer patients. J Gastrointest Surg. 2017;21:543–53.
Ghaferi AA, Birkmeyer JD, Dimick JB. Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Ann Surg. 2009;250:1029–34.
Xu Z, Mohile SG, Tejani MA, et al. Poor compliance with adjuvant chemotherapy use associated with poorer survival in patients with rectal cancer: an NCDB analysis. Cancer Am Cancer Soc. 2017;123:52–61.
Aquina CT, Becerra AZ, Justiniano CF, et al. Surgeon, hospital, and geographic variation in minimally invasive colectomy. Ann Surg. 2019;269:1109–16.
Kim Y, Steiner PM. Causal graphical views of fixed-effects and random-effects models. Br J Math Stat Psychol. 2021;74:165–83.
Hadfield JD. MCMC methods for multi-response generalized linear mixed models: the MCMCglmm R package. J. Stat. Softw.. 2010;33:22.
Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q. 1966;44(Suppl):166–206.
Saver BG, Martin SA, Adler RN, et al. Care that matters: quality measurement and health care. PLoS Med. 2015;12:e1001902.
Sweigert PJ, Eguia E, Baker MS, et al. Assessment of textbook oncologic outcomes following pancreaticoduodenectomy for pancreatic adenocarcinoma. J Surg Oncol. 2020;121:936–44.
Lingsma HF, Bottle A, Middleton S, Kievit J, Steyerberg EW, Marang-van de Mheen PJ. Evaluation of hospital outcomes: the relation between length-of-stay, readmission, and mortality in a large international administrative database. BMC Health Serv Res. 2018;18:116.
Dimick JB, Staiger DO, Osborne NH, Nicholas LH, Birkmeyer JD. Composite measures for rating hospital quality with major surgery. Health Serv Res. 2012;47:1861–79.
Marang-van de Mheen PJ, Dijs-Elsinga J, Otten W, et al. The relative importance of quality of care information when choosing a hospital for surgical treatment: a hospital choice experiment. Med Decis Making. 2011;31:816–27.
Wiseman JT, Abdel-Misih S, Beal EW, et al. A multi-institutional analysis of textbook outcomes among patients undergoing cytoreductive surgery for peritoneal surface malignancies. Surg Oncol. 2020;37:101492.
Merath K, Chen Q, Bagante F, et al. A Multi-institutional international analysis of textbook outcomes among patients undergoing curative-intent resection of intrahepatic cholangiocarcinoma. JAMA Surg. 2019;154:e190571.
van Roessel S, Mackay TM, van Dieren S, et al. Textbook outcome: nationwide analysis of a novel quality measure in pancreatic surgery. Ann Surg. 2020;271:155–62.
Heidsma CM, Hyer M, Tsilimigras DI, et al. Incidence and impact of textbook outcome among patients undergoing resection of pancreatic neuroendocrine tumors: results of the US Neuroendocrine Tumor Study Group. J Surg Oncol. 2020;121:1201–8.
Sweigert PJ, Eguia E, Baker MS, et al. Assessment of Cancer Center Variation in textbook oncologic outcomes following colectomy for adenocarcinoma. J Gastrointest Surg. 2021;25:775–85.
Wiseman JT, Ethun CG, Cloyd JM, et al. Analysis of textbook outcomes among patients undergoing resection of retroperitoneal sarcoma: a multi-institutional analysis of the US Sarcoma Collaborative. J Surg Oncol. 2020;122:1189–98.
Hobeika C, Fuks D, Cauchy F, et al. Benchmark performance of laparoscopic left lateral sectionectomy and right hepatectomy in expert centers. J Hepatol. 2020;73:1100–8.
Denbo J, Anaya DA. Textbook outcomes following liver resection for cancer: a new standard for quality benchmarking and patient decision-making. Ann Surg Oncol. 2020;27:3118–20.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Virtual forum session oral presentation at the Society of Surgical Oncology 2021 International Conference on Surgical Cancer Care on March 18th, 2021.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Aquina, C.T., Hamad, A., Becerra, A.Z. et al. Is Textbook Oncologic Outcome a Valid Hospital-Quality Metric after High-Risk Surgical Oncology Procedures?. Ann Surg Oncol 28, 8028–8045 (2021). https://doi.org/10.1245/s10434-021-10478-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10478-0