Abstract
Background
Although laparoscopic distal pancreatectomy (LDP) versus open approaches (ODP) for pancreatic adenocarcinoma (PDAC) is associated with reduced morbidity, its impact on optimal adjuvant chemotherapy (AC) utilization remains unclear. Furthermore, it is uncertain whether oncologic resection quality markers are equivalent between approaches.
Methods
The National Cancer Database (NCDB) was queried between 2010 and 2016 for PDAC patients undergoing DP. Effect of LDP vs ODP and institutional case volumes on margin status, hospital stay, 30-day and 90-day mortality, administration of and delay to AC, and 30-day unplanned readmission were analyzed using binary and linear logistic regression. Cox multivariable regression was used to correct for confounders.
Results
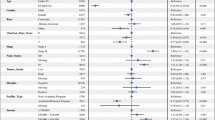
The search yielded 3411 patients; 996 (29.2%) had LDP and 2415 (70.8%) had ODP. ODP had higher odds of readmission [odds ratio (OR) 1.681, p = 0.01] and longer hospital stay [β 1.745, p = 0.004]. No difference was found for 30-day mortality [OR 1.689, p = 0.303], 90-day mortality [OR 1.936, p = 0.207], and overall survival [HR 1.231, p = 0.057]. The highest-volume centers had improved odds of AC [OR 1.275, p = 0.027] regardless of approach. LDP conferred lower margin positivity [OR 0.581, p = 0.005], increased AC use [3rd quartile: OR 1.844, p = 0.026; 4th quartile; OR 2.144, p = 0.045], and fewer AC delays [4th quartile: OR 0.786, p = 0.045] in higher-volume centers.
Conclusions
In selected patients, LDP offers an oncologically safe alternative to ODP for PDAC independent of institutional volume. However, additional oncologic benefit due to optimal AC utilization and lower positive margin rates in higher volume centers suggests that LDP by experienced teams can achieve best possible cancer outcomes.


Similar content being viewed by others
References
Riviere D, Gurusamy KS, Kooby DA, et al. Laparoscopic versus open distal pancreatectomy for pancreatic cancer. Cochrane Database Syst Rev. Apr 4 2016;4:Cd011391.
Joliat GR, Demartines N, Halkic N, Petermann D, Schafer M. Short-term outcomes after distal pancreatectomy: laparotomy vs laparoscopy—a single-center series. Ann Med Surg (Lond). 2017;13:1–5.
van Hilst J, de Rooij T, Klompmaker S, et al. Minimally Invasive versus open distal pancreatectomy for ductal adenocarcinoma (DIPLOMA): a Pan-European propensity score matched study. Ann Surg. 2019;269(1):10–7.
Björnsson B, Larsson AL, Hjalmarsson C, Gasslander T, Sandström P. Comparison of the duration of hospital stay after laparoscopic or open distal pancreatectomy: randomized controlled trial. Br J Surg. 2020;107:1281–2188.
Zhang Y, Chen XM, Sun DL. Laparoscopic versus open distal pancreatectomy: a single-institution comparative study. World J Surg Oncol. 2014;12:327.
Stauffer JA, Coppola A, Mody K, Asbun HJ. Laparoscopic versus open distal pancreatectomy for pancreatic adenocarcinoma. World J Surg. 2016;40(6):1477–84.
Jarufe N, Soto P, Ahumada V, et al. Laparoscopic versus open distal pancreatectomy: comparative analysis of clinical outcomes at a single institution. Surg Laparosc Endosc Percutan Tech. 2018;28(1):62–6.
Gavriilidis P, Roberts KJ, Sutcliffe RP. Laparoscopic versus open distal pancreatectomy for pancreatic adenocarcinoma: a systematic review and meta-analysis. Acta Chir Belg. 2018;118(5):278–86.
de Rooij T, van Hilst J, van Santvoort H, et al. Minimally invasive versus open distal pancreatectomy (LEOPARD): a multicenter patient-blinded randomized controlled trial. Ann Surg. 2019;269(1):2–9.
Bauman MD, Becerra DG, Kilbane EM, et al. Laparoscopic distal pancreatectomy for pancreatic cancer is safe and effective. Surg Endosc. 2018;32(1):53–61.
Kooby DA, Gillespie T, Bentrem D, et al. Left-sided pancreatectomy: a multicenter comparison of laparoscopic and open approaches. Ann Surg. 2008;248(3):438–46.
Zhang AB, Wang Y, Hu C, Shen Y, Zheng SS. Laparoscopic versus open distal pancreatectomy for pancreatic ductal adenocarcinoma: a single-center experience. J Zhejiang Univ Sci B. 2017;18(6):532–8.
Lee SY, Allen PJ, Sadot E, et al. Distal pancreatectomy: a single institution’s experience in open, laparoscopic, and robotic approaches. J Am Coll Surg. 2015;220(1):18–27.
Kantor O, Bryan DS, Talamonti MS, et al. Laparoscopic distal pancreatectomy for cancer provides oncologic outcomes and overall survival identical to open distal pancreatectomy. J Gastrointest Surg. 2017;21(10):1620–5.
Anderson KL Jr, Adam MA, Thomas S, Roman SA, Sosa JA. Impact of minimally invasive vs. open distal pancreatectomy on use of adjuvant chemoradiation for pancreatic adenocarcinoma. Am J Surg. 2017;213(4):601–5.
Korrel M, Lof S, van Hilst J, et al. Predictors for survival in an international cohort of patients undergoing distal pancreatectomy for pancreatic ductal adenocarcinoma. Ann Surg Oncol. 2020;28:1079–87.
Ma SJ, Oladeru OT, Miccio JA, Iovoli AJ, Hermann GM, Singh AK. Association of timing of adjuvant therapy with survival in patients with resected stage I to II pancreatic cancer. JAMA Netw Open. 2019;2(8):e199126–e199126.
White RJ, Hasan S, Monga D, et al. Time to adjuvant systemic therapy following pancreatic cancer resection and effect on outcome. Pancreas. Sep 2019;48(8):1086–91.
Demir IE, Jäger C, Schlitter AM, et al. R0 versus R1 resection matters after pancreaticoduodenectomy, and less after distal or total pancreatectomy for pancreatic cancer. Ann Surg. 2018;268(6):1058–68.
Brennan MF, Kattan MW, Klimstra D, Conlon K. Prognostic nomogram for patients undergoing resection for adenocarcinoma of the pancreas. Ann Surg. 2004;240(2):293–8.
Raut CP, Tseng JF, Sun CC, et al. Impact of resection status on pattern of failure and survival after pancreaticoduodenectomy for pancreatic adenocarcinoma. Ann Surg. 2007;246(1):52–60.
Menon KV, Gomez D, Smith AM, Anthoney A, Verbeke CS. Impact of margin status on survival following pancreatoduodenectomy for cancer: the Leeds Pathology Protocol (LEEPP). HPB (Oxf). 2009;11(1):18–24.
Plotkin A, Ceppa EP, Zarzaur BL, Kilbane EM, Riall TS, Pitt HA. Reduced morbidity with minimally invasive distal pancreatectomy for pancreatic adenocarcinoma. HPB (Oxford). 2017;19(3):279–85.
Raoof M, Ituarte PHG, Woo Y, et al. Propensity score-matched comparison of oncological outcomes between laparoscopic and open distal pancreatic resection. Br J Surg. 2018;105(5):578–86.
Adam MA, Choudhury K, Goffredo P, et al. Minimally invasive distal pancreatectomy for cancer: short-term oncologic outcomes in 1,733 patients. World J Surg. 2015;39(10):2564–72.
Lemmens VE, Bosscha K, van der Schelling G, Brenninkmeijer S, Coebergh JW, de Hingh IH. Improving outcome for patients with pancreatic cancer through centralization. Br J Surg. 2011;98(10):1455–62.
Funding
This research did not receive any specific funding from agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None of the authors have declared any conflicts of interest. Claudius Conrad—Consultant for Fuji, Integra and Olympus
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Salehi, O., Vega, E.A., Kutlu, O. . et al. Does a Laparoscopic Approach to Distal Pancreatectomy for Cancer Contribute to Optimal Adjuvant Chemotherapy Utilization?. Ann Surg Oncol 28, 8273–8280 (2021). https://doi.org/10.1245/s10434-021-10241-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10241-5