Abstract
Background
The utility of sentinel lymph node biopsy (SLNB) for non-ulcerated T1b melanoma is debated and associated costs are poorly characterized. Prior work using institutional registries may overestimate the incidence of nodal positivity in this population.
Objective
The aim of this study was to estimate the use of SLNB, positivity prevalence, and procedural costs in patients with non-ulcerated T1b melanoma using a population-based registry.
Methods
We identified patients with clinically node-negative, non-ulcerated melanoma 0.8–1.0 mm thick (T1b according to the 8th edition standard of the American Joint Committee on Cancer) in the Surveillance, Epidemiology, and End Results database from 2010 to 2016. The prevalence of SLNB procedures and positive sentinel nodes were calculated. Factors associated with SLNB and sentinel node positivity were assessed using logistic regression. Medicare reimbursement costs and patient out-of-pocket expenses for SLNB and wide local excision (WLE) versus WLE alone were estimated.
Results
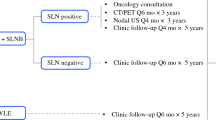
Among 7245 included patients, 3835(53%) underwent SLNB, 156 (4.1%, 95% confidence interval 3.5–4.7) of whom had a positive SLNB. Younger age, >1 mitosis per mm2, female sex, and truncal tumor location were associated with higher odds of positivity. The estimated SLNB cost to identify one patient with stage III disease was $71,700 (range $54,648–$83,172). Out-of-pocket expenses for a Medicare patient were estimated to be $652 for a WLE and SLNB and $79 for a WLE alone.
Conclusions
In this population-based study, only 4% of selected non-ulcerated T1b patients had a positive SLNB, which is lower than prior reports. At the population level, SLNB is associated with high costs per prognostic information gained.

Similar content being viewed by others
References
Morton DL, Thompson JF, Cochran AJ, et al. Final trial report of sentinel-node biopsy versus nodal observation in melanoma. N Engl J Med. 2014;370(7):599–609. https://doi.org/10.1056/NEJMoa1310460.
Clinical Practice Guidelines in Oncology: Cutaneous Melanoma. National comprehensive cancer network. 2019. Available at: https://www.nccn.org/professionals/physician_gls/pdf/cutaneous_melanoma_blocks.pdf. Accessed 30 Sep 2019.
Cordeiro E, Gervais MK, Shah PS, Look Hong NJ, Wright FC. Sentinel lymph node biopsy in thin cutaneous melanoma: a systematic review and meta-analysis. Ann Surg Oncol. 2016;23(13):4178–88. https://doi.org/10.1245/s10434-016-5137-z.
Han D, Yu D, Zhao X, et al. Sentinel node biopsy is indicated for thin melanomas ≥ 0. 76 mm. Ann Surg Oncol. 2012;19(11):3335–42.
Han D, Zager JS, Shyr Y, et al. Clinicopathologic predictors of sentinel lymph node metastasis in thin melanoma. J Clin Oncol. 2013;31(35):4387–93. https://doi.org/10.1200/JCO.2013.50.1114.
Hershko D, Robb B, Lowy A, et al. Sentinel lymph node biopsy in thin melanoma patients. J Surg Oncol. 2006;93:279–85.
Balch CM, Thompson JF, Gershenwald JE, et al. Age as a predictor of sentinel node metastasis among patients with localized melanoma: an inverse correlation of melanoma mortality and incidence of sentinel node metastasis among young and old patients. Ann Surg Oncol. 2014;21(4):1075–81. https://doi.org/10.1245/s10434-013-3464-x.
Bartlett EK, Gimotty PA, Sinnamon AJ, et al. Clark level risk stratifies patients with mitogenic thin melanomas for sentinel lymph node biopsy. Ann Surg Oncol. 2014;21(2):643–9. https://doi.org/10.1245/s10434-013-3313-y.
Cavanaugh-Hussey MW, Mu EW, Kang S, Balch CM, Wang T. Older age is associated with a higher incidence of melanoma death but a lower incidence of sentinel lymph node metastasis in the seer databases (2003–2011). Ann Surg Oncol. 2015;22(7):2120–6. https://doi.org/10.1245/s10434-015-4538-8.
Egger ME, Stevenson M, Bhutiani N, et al. Should sentinel lymph node biopsy be performed for all T1b melanomas in the new 8 th edition american joint committee on cancer staging system. J Am Coll Surg. 2019;228(4):466–72.
Starz H, Balda BR. Benefit of sentinel lymphadenectomy for patients with nonulcerated cutaneous melanomas in the Breslow range between and 1 mm: a follow-up study of 148 patients. Int J Cancer. 2007;121(3):689–93. https://doi.org/10.1002/ijc.22707.
Ranieri JM, Wagner JD, Wenck S, Johnson CS, Coleman JJ. The prognostic importance of sentinel lymph node biopsy in thin melanoma. Ann Surg Oncol. 2006;13(7):927–32. https://doi.org/10.1245/ASO.2006.04.023.
Vermeeren L, Van der Ent F, Sastrowijoto P, Hulsewé K. Sentinel lymph node biopsy in patients with thin melanoma: occurrence of nodal metastases and its prognostic value. Eur J Dermatol. 2010;20(1):30–4.
Sinnamon AJ, Gimotty PA, Karakousis GC, Yang YX. Survival outcomes following lymph node biopsy in thin melanoma—a propensity-matched analysis. Ann Surg Oncol. 2021;28(3):1634–41. https://doi.org/10.1245/s10434-020-08997-3.
Mallin K, Browner A, Palis B, et al. Incident cases captured in the national cancer database compared with those in US population based central cancer registries in 2012–2014. Ann Surg Oncol. 2019;26(6):1604–12. https://doi.org/10.1245/s10434-019-07213-1.
Sondak VK, Messina JL, Zager JS. Selecting patients with thin melanoma for sentinel lymph node biopsy – this time it’s personal. JAMA Dermatol. 2017;153(9):857–8. https://doi.org/10.1001/jamadermatol.2017.2496.
Serra-Arbeloa P, Rabines-Juarez A, Alvarez-Ruiz M, Guillen-Grima F. Sentinel node biopsy in patients with primary cutaneous melanoma of any thickness: a cost-effectiveness analysis. Sugical Oncol. 2016;25:205–11.
Agnese DM, Abdessalam SF, Burak WE, et al. Cost-effectiveness of sentinel lymph node biopsy in thin melanomas. Surgery. 2003;134(4):542–7. https://doi.org/10.1016/S0039-6060(03)00275-7.
Hu Y, Briggs A, Gennarelli RL, et al. Sentinel lymph node biopsy for t1b melanoma: balancing prognostic value and cost. Ann Surg Oncol. 2020;27(13):5248–56. https://doi.org/10.1245/s10434-020-08558-8.
Overview of the SEER Program. National Cancer Institute Surveillance, Epidemiology, and End Resuls Program. 2019. Available at: https://seer.cancer.gov/about/overview.html. Accessed 2 Jul 2020.
Centers for Medicare and Medicaid Services (CMS). Medicare. Baltimore, MD.
Centers for Medicare and Medicaid Services (CMS). Medicare Costs at a Glance. Baltimore, MD.
Brown LD, Cai TT, Dasgupta A. Interval estimation for a binomial proportion. Stat Sci. 2001;16:101–33.
Cockburn M, Swetter SM, Peng D, Keegan THM, Deapen D, Clarke CA. Melanoma underreporting: why does it happen, how big is the problem, and how do we fix it? J Am Acad Dermatol. 2008;59(6):1081–5. https://doi.org/10.1016/j.jaad.2008.08.007.
Hall HI, Jamison P, Fulton JP, Clutter G, Roffers S, Parrish P. Reporting cutaneous melanoma to cancer registries in the United States. J Am Acad Dermatol. 2003;49(4):624–30. https://doi.org/10.1067/S0190-9622(03)00885-5.
Sinnamon AJ, Neuwirth MG, Yalamanchi P, et al. Association between patient age and lymph node positivity in thin melanoma. JAMA Dermatol. 2017;153(9):866–73. https://doi.org/10.1001/jamadermatol.2017.2497.
Merlino LA, Sullivan KJ, Whitaker DC, Lynch CF. The independent pathology laboratory as a reporting source for cutaneous melanoma incidence in Iowa, 1977–1994. J Am Acad Dermatol. 1997;37(4):578–85. https://doi.org/10.1016/S0190-9622(97)70175-0.
Koh HK, Clapp RW, Barnett JM, et al. Systematic underreporting of cutaneous malignant melanoma in massachusetts: possible implications for national incidence figures. J Am Acad Dermatol. 1991;24(4):545–50. https://doi.org/10.1016/0190-9622(91)70079-H.
Tejera-Vaquerizo A, Pérez-Cabello G, Marínez-Leborans L, et al. Is mitotic rate still useful in the management of patients with thin melanoma? J Eur Acad Dermatology Venereol. 2017;31(12):2025–9. https://doi.org/10.1111/jdv.14485.
Durham AB, Schwartz JL, Lowe L, et al. The natural history of thin melanoma and the utility of sentinel lymph node biopsy. J Surg Oncol. 2017;116(8):1185–92. https://doi.org/10.1002/jso.24765.
Kesmodel SB, Karakousis GC, Botbyl JD, et al. Mitotic rate as a predictor of sentinel lymph nodepositivity in patients with thin melanomas. Ann Surg Oncol. 2005;12(6):449–58. https://doi.org/10.1245/ASO.2005.04.027.
Singleterry J. The Costs of Cancer: Addressing Patient Costs; 2017. doi:https://doi.org/10.1007/BF00300534
Gabel J, Whitmore H, Green M, Stromberg S, Oran R. Consumer Cost-Sharing in Marketplace vs. Employer Health Insurance Plans, 2015. Available at: https://www.commonwealthfund.org/publications/issue-briefs/2015/dec/consumer-cost-sharing-marketplace-vs-employer-health-insurance.
Zafar SY, Peppercorn JM, Schrag D, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 2013;18(4):381–90. https://doi.org/10.1634/theoncologist.2012-0279.
Chino F, Peppercorn J, Rushing C, et al. Out-of-pocket costs, financial distress, and underinsurance in cancer care. JAMA Oncol. 2017;3(11):1582–4. https://doi.org/10.1001/jamaoncol.2016.
Allcott N, Dunham L, Levy D, Carr J, Stitzenberg K. Financial burden amongst cancer patients treated with curative intent surgery alone. Am J Surg. 2019;218(3):452–6.
Medicare Geographic Variation. Centers for Medicare and Medicaid Services. 2019. Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Geographic-Variation. Accessed 6 Apr 2020.
Lopez E, Neuman T, Jacobson G, Levitt L. How Much More Than Medicare Do Private Insurers Pay? A Review of the Literature. 2020.
Acknowledgment
Joshua N. Herb, David W. Ollila, Karyn B. Stitzenberg, and Michael O. Meyers have no commercial interests to report. Joshua N. Herb is supported by a National Research Service Award Pre-Doctoral/Post-Doctoral Traineeship from the Agency for Healthcare Research and Quality sponsored by the Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, Grant No. 5T32 HS000032.
Funding
Joshua N. Herb is supported by a National Research Service Award Pre-Doctoral/Post-Doctoral Traineeship from the Agency for Healthcare Research and Quality sponsored by the Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, Grant No. 5T32 HS000032.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Herb, J.N., Ollila, D.W., Stitzenberg, K.B. et al. Use and Costs of Sentinel Lymph Node Biopsy in Non-Ulcerated T1b Melanoma: Analysis of a Population-Based Registry. Ann Surg Oncol 28, 3470–3478 (2021). https://doi.org/10.1245/s10434-021-09998-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-09998-6