Abstract
Background
Robotic surgery has been widely adopted for complex procedures to overcome technical limitations of open or laparoscopic methods. However, evidence of any subsequent benefit is lacking. This study was undertaken to compare open, laparoscopic, and robotic gastrectomy in technically demanding procedure—D2 dissection in obese patients with gastric cancer.
Methods
Data collected between 2010 and 2018 on D2 gastrectomy in obese patients with gastric cancer were used to conduct retrospective analysis, comparing short- and long-term outcomes of open, laparoscopic, and robotic techniques.
Results
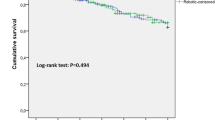
In a total of 185 patients, there were 69 open, 62 laparoscopic, and 54 robotic gastrectomy procedures. Median ages for respective surgical groups were 66 (interquartile range [IQR]: 61–64 years), 63 (IQR: 59–63), and 59 years (IQR: 56–60 years) (p = 0.009). Early-stage gastric cancer ranked proportionately higher in the laparoscopic group (p = 0.005), but operative times were similar among groups. Estimated blood loss (p < 0.001) and drainage volumes (p = 0.001) were higher in the open group, relative to others. Although a robotic approach performed best in overall compliance and in mean number of retrieved lymph node, observed rates of early or late complications did not differ by technique. The open group experienced significantly poorer overall (p = 0.039) and relapse-free (p < 0.001) survival compared with the laparoscopic or robotic group. Robotic surgery emerged from multivariable Cox regression as a protective factor for relapse-free survival (HR = 0.314, 95% CI 0.116–0.851).
Conclusions
In obese patients with gastric cancer, robotic gastrectomy with D2 lymphadenectomy proved comparable to open or laparoscopic technique short-term, yielding better long-term outcomes.


Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Fujitani K, Yang HK, Mizusawa J, et al. Gastrectomy plus chemotherapy versus chemotherapy alone for advanced gastric cancer with a single non-curable factor (REGATTA): a phase 3, randomised controlled trial. Lancet Oncol. 2016;17:309–18.
Kim HH, Han SU, Kim MC, et al. Effect of laparoscopic distal gastrectomy vs open distal gastrectomy on long-term survival among patients with stage I gastric cancer: the KLASS-01 randomized clinical trial. JAMA Oncol. 2019;5:506–13.
Hyung WJ, Yang HK, Park YK, et al. Long-term outcomes of laparoscopic distal gastrectomy for locally advanced gastric cancer: the KLASS-02-RCT randomized clinical trial. J Clin Oncol. 2020;38:3304–13.
Inaki N, Etoh T, Ohyama T, et al. A Multi-institutional, Prospective, Phase II Feasibility Study of Laparoscopy-Assisted Distal Gastrectomy with D2 Lymph Node Dissection for Locally Advanced Gastric Cancer (JLSSG0901). World J Surg. 2015;39:2734–41.
Lee J, Kim YM, Woo Y, Obama K, Noh SH, Hyung WJ. Robotic distal subtotal gastrectomy with D2 lymphadenectomy for gastric cancer patients with high body mass index: comparison with conventional laparoscopic distal subtotal gastrectomy with D2 lymphadenectomy. Surg Endosc. 2015;29:3251–60.
Obama K, Sakai Y. Current status of robotic gastrectomy for gastric cancer. Surg Today. 2016;46:528–34.
Woo Y, Hyung WJ, Pak KH, et al. Robotic gastrectomy as an oncologically sound alternative to laparoscopic resections for the treatment of early-stage gastric cancers. Arch Surg. 2011;146:1086–92.
Ye SP, Shi J, Liu DN, et al. Robotic- versus laparoscopic-assisted distal gastrectomy with D2 lymphadenectomy for advanced gastric cancer based on propensity score matching: short-term outcomes at a high-capacity center. Sci Rep. 2020;10:6502.
Yang C, Shi Y, Xie S, et al. Short-term outcomes of robotic- versus laparoscopic-assisted Total Gastrectomy for advanced gastric Cancer: a propensity score matching study. BMC Cancer. 2020;20:669.
Alhossaini RM, Altamran AA, Cho M, et al. Lower rate of conversion using robotic-assisted surgery compared to laparoscopy in completion total gastrectomy for remnant gastric cancer. Surg Endosc. 2020;34:847–52.
Son T, Lee JH, Kim YM, Kim HI, Noh SH, Hyung WJ. Robotic spleen-preserving total gastrectomy for gastric cancer: comparison with conventional laparoscopic procedure. Surg Endosc. 2014;28:2606–15.
Kim YW, Reim D, Park JY, et al. Role of robot-assisted distal gastrectomy compared to laparoscopy-assisted distal gastrectomy in suprapancreatic nodal dissection for gastric cancer. Surg Endosc. 2016;30:1547–52.
Kim KM, An JY, Kim HI, Cheong JH, Hyung WJ, Noh SH. Major early complications following open, laparoscopic and robotic gastrectomy. Br J Surg. 2012;99:1681–7.
Yang SY, Roh KH, Kim YN, et al. Surgical outcomes after open, laparoscopic, and robotic gastrectomy for gastric cancer. Ann Surg Oncol. 2017;24:1770–7.
Guner A, Kim SY, Yu JE, et al. Parameters for predicting surgical outcomes for gastric cancer patients: simple is better than complex. Ann Surg Oncol. 2018;25:3239–47.
Kwon IG, Son T, Kim HI, Hyung WJ. Fluorescent lymphography-guided lymphadenectomy during robotic radical gastrectomy for gastric cancer. JAMA Surg. 2019;154:150–8.
Japanese Gastric Cancer A. Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer. 2020. https://doi.org/10.1007/s10120-020-01042-y
Guideline Committee of the Korean Gastric Cancer Association DWG, Review P. Korean Practice Guideline for Gastric Cancer 2018: an evidence-based, multi-disciplinary approach. J Gastric Cancer. 2019;19:1–48
Edge SB, Edge SB. AJCC Cancer Staging Manual. 8th edn. Berlin: Springer; 2017.
de Steur WO, Hartgrink HH, Dikken JL, Putter H, van de Velde CJ. Quality control of lymph node dissection in the Dutch Gastric Cancer Trial. Br J Surg. 2015;102:1388–93.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Song J, Lee HJ, Cho GS, et al. Recurrence following laparoscopy-assisted gastrectomy for gastric cancer: a multicenter retrospective analysis of 1,417 patients. Ann Surg Oncol. 2010;17:1777–86.
Park JY, Ryu KW, Reim D, et al. Robot-assisted gastrectomy for early gastric cancer: is it beneficial in viscerally obese patients compared to laparoscopic gastrectomy? World J Surg. 2015;39:1789–97.
Miyaki A, Imamura K, Kobayashi R, Takami M, Matsumoto J. Impact of visceral fat on laparoscopy-assisted distal gastrectomy. Surgeon. 2013;11:76–81.
Ueda J, Ichimiya H, Okido M, Kato M. The impact of visceral fat accumulation on laparoscopy-assisted distal gastrectomy for early gastric cancer. J Laparoendosc Adv Surg Tech A. 2009;19:157–62.
Claassen YHM, de Steur WO, Hartgrink HH, et al. Surgicopathological quality control and protocol adherence to lymphadenectomy in the CRITICS Gastric Cancer Trial. Ann Surg. 2018;268:1008–13.
Lin GT, Chen QY, Zhong Q, et al. Intraoperative surrogate indicators of gastric cancer patients’ long-term prognosis: the number of lymph nodes examined relates to the lymph node noncompliance rate. Ann Surg Oncol. 2020;27:3281–93.
Lin GT, Chen QY, Zheng CH, et al. Lymph node noncompliance affects the long-term prognosis of patients with gastric cancer after laparoscopic total gastrectomy. J Gastrointest Surg. 2020;24:540–50.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2019R1H1A2079953).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Seohee Choi, Jeong Ho Song, Sejin Lee, Minah Cho, Yoo Min Kim, Hyoung-Il Kim have no conflicts of interest or financial ties to disclose. Dr. Woo Jin Hyung received research grants from Medtronic and GC Pharma. These funding sources did not influence our study design and played no part in its execution, analytics, and data interpretation or in our decision to submit results.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Choi, S., Song, J.H., Lee, S. et al. Surgical Merits of Open, Laparoscopic, and Robotic Gastrectomy Techniques with D2 Lymphadenectomy in Obese Patients with Gastric Cancer. Ann Surg Oncol 28, 7051–7060 (2021). https://doi.org/10.1245/s10434-021-09952-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-09952-6