Abstract
Background
We have previously demonstrated that implementing an enhanced recovery protocol (ERP) improved outcomes after esophagectomy. We sought to examine if, after a decade of an established ERP, further improvements in postoperative outcomes could be made after continually optimizing and revising the pathway.
Methods
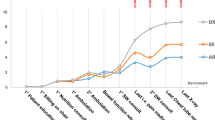
Patients undergoing esophagectomy for cancer from January 2019 to January 2020 were compared with our early-experience group within the initial ERP (June 2010–May 2011) and pre-ERP traditional care (June 2009–May 2010). The original ERP was initiated on June 2010 and underwent several revisions from 2014 to 2018, incorporating the following, amongst other elements: shorten the planned length of stay from 7 to 6 days, elimination of nasogastric tubes, use of soft closed-suction chest drains, and increased application of minimally invasive esophagectomy (MIE). Thirty-day outcomes (complications, length of stay, readmission) were compared for patients undergoing esophagectomy during the initial and most recent ERPs.
Results
Overall, 175 patients were identified; 47 underwent esophagectomy before ERP implementation (traditional care), 59 patients underwent esophagectomy after implementation of the original ERP, and 69 patients underwent esophagectomy after the most recent ERP (ERP 2.0). The groups were similar with respect to age, sex, and diagnosis. There were three times more MIEs in the ERP 2.0 group with a shorter median length of stay (7 [6–9] vs. 8 [7–17] vs. 10 [9–17]; p < 0.001) without impacting postoperative morbidity or readmission rate.
Conclusion
Continued evaluation of institutional outcomes after esophagectomy should be performed to identify target areas for optimization and revision of established enhanced recovery protocols. ERPs are dynamic processes that can be further refined to yield greater improvements in outcomes.
Similar content being viewed by others
References
Kehlet H, Mogensen T. Hospital stay of 2 days after open sigmoidectomy with a multimodal rehabilitation programme. Br J Surg. 1999;86(2):227–30.
Glaser G, Dowdy SC, Peedicayil A. Enhanced recovery after surgery in gynecologic oncology. Int J Gynaecol Obstet. 2018;143(Suppl 2):143–6.
Lassen K, Coolsen MM, Slim K, et al. Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS®) society recommendations. Clin Nutr. 2012;31(6):817–30.
Gustafsson UO, Scott MJ, Schwenk W, et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS®) SOCIETY recommendations. World J Surg. 2013;37(2):259–84.
Nygren J, Thacker J, Carli F, et al. Guidelines for perioperative care in elective rectal/pelvic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Clin Nutr. 2012;31(6):801–16.
Eustache J, Ferri LE, Feldman LS, Lee L, Spicer JD. Enhanced recovery after pulmonary surgery. J Thorac Dis. 2018;10(Suppl 32):S3755–60.
Ban KA, Berian JR, Liu JB, Ko CY, Feldman LS, Thacker JKM. Effect of diagnosis on outcomes in the setting of enhanced recovery protocols. Dis Colon Rectum. 2018;61(7):847–53.
Low DE, Allum W, De Manzoni G, et al. Guidelines for perioperative care in esophagectomy: Enhanced Recovery After Surgery (ERAS®) society recommendations. World J Surg. 2019;43(2):299–330.
Cerfolio RJ, Bryant AS, Bass CS, Alexander JR, Bartolucci AA. Fast tracking after Ivor Lewis esophagogastrectomy. Chest. 2004;126(4):1187–94.
Li C, Ferri LE, Mulder DS, et al. An enhanced recovery pathway decreases duration of stay after esophagectomy. Surgery. 2012;152(4):606–14 (discussion 14-6).
Seely AJ, Ivanovic J, Threader J, et al. Systematic classification of morbidity and mortality after thoracic surgery. Ann Thorac Surg. 2010;90(3):936–42 (discussion 42).
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Minnella EM, Awasthi R, Loiselle SE, Agnihotram RV, Ferri LE, Carli F. Effect of exercise and nutrition prehabilitation on functional capacity in esophagogastric cancer surgery: a randomized clinical trial. JAMA Surg. 2018;153(12):1081–9.
Cools-Lartigue J, Andalib A, Abo-Alsaud A, et al. Routine contrast esophagram has minimal impact on the postoperative management of patients undergoing esophagectomy for esophageal cancer. Ann Surg Oncol. 2014;21(8):2573–9.
Mistry RC, Vijayabhaskar R, Karimundackal G, Jiwnani S, Pramesh CS. Effect of short-term vs prolonged nasogastric decompression on major postesophagectomy complications: a parallel-group, randomized trial. Arch Surg. 2012;147(8):747–51.
Carroll PA, Yeung JC, Darling GE. Elimination of routine feeding jejunostomy after esophagectomy. Ann Thorac Surg. 2020;110(5):1706–13.
Varghese TK Jr, Wood DE, Farjah F, et al. Variation in esophagectomy outcomes in hospitals meeting Leapfrog volume outcome standards. Ann Thorac Surg. 2011;91(4):1003–9 (discussion 9-10).
Low DE, Alderson D, Cecconello I, et al. International consensus on standardization of data collection for complications associated with esophagectomy: Esophagectomy Complications Consensus Group (ECCG). Ann Surg. 2015;262(2):286–94.
Triantafyllou T, Olson MT, Theodorou D, Schizas D, Singhal S. Enhanced recovery pathways vs standard care pathways in esophageal cancer surgery: systematic review and meta-analysis. Esophagus. 2020;17(2):100–12.
Weijs TJ, Kumagai K, Berkelmans GH, Nieuwenhuijzen GA, Nilsson M, Luyer MD. Nasogastric decompression following esophagectomy: a systematic literature review and meta-analysis. Dis Esophagus. 2017;30(3):1–8.
Shackcloth MJ, McCarron E, Kendall J, et al. Randomized clinical trial to determine the effect of nasogastric drainage on tracheal acid aspiration following oesophagectomy. Br J Surg. 2006;93(5):547–52.
Reynolds JV, Donlon N, Elliott JA, et al. Comparison of Esophagectomy outcomes between a National Center, a National Audit Collaborative, and an International database using the Esophageal Complications Consensus Group (ECCG) standardized definitions. Dis Esophagus. 2021;34(1):doaa060.
Mariette C, Markar SR, Dabakuyo-Yonli TS, et al. Hybrid minimally invasive esophagectomy for esophageal cancer. N Engl J Med. 2019;380(2):152–62.
Biere SS, van Berge Henegouwen MI, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet. 2012;379(9829):1887–92.
Seesing MFJ, Gisbertz SS, Goense L, et al. A propensity score matched analysis of open versus minimally invasive transthoracic esophagectomy in the Netherlands. Ann Surg. 2017;266(5):839–46.
Funding
This study did not receive any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Yehonatan Nevo, Sarah Arjah, Amit Katz, Jose Ramirez Garcia Luna, Jonathan Spicer, Jonathan Cools-Lartigue, Carmen Muller, Liane Feldman, and Lorenzo Ferri have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nevo, Y., Arjah, S., Katz, A. et al. ERAS 2.0: Continued Refinement of an Established Enhanced Recovery Protocol for Esophagectomy. Ann Surg Oncol 28, 4850–4858 (2021). https://doi.org/10.1245/s10434-021-09854-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-09854-7