Abstract
Background
Longer time to surgery worsens survival in multiple malignancies, including lung, colorectal, and breast cancers, but limited data exist for well-differentiated thyroid cancer. We sought to investigate the impact of time to surgery on overall survival in patients with papillary thyroid cancer.
Methods
In a retrospective cohort study of the National Cancer Database, we used Cox proportional hazard models to investigate overall survival as a function of time between diagnosis and surgery for adults with papillary thyroid cancer, adjusting for demographic, patient, and cancer-related variables. Time to surgery was investigated both as a continuous variable and as intervals of 0–90 days, 90–180 days, and > 180 days. Subgroup analyses were conducted by T stage.
Results
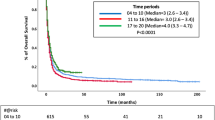
Overall, 103,812 adults with papillary thyroid cancer were included from 2004 to 2016. Median follow-up was 55.2 months (interquartile range 28.4–89.5). Increasing time to surgery was associated with increased mortality: delaying by 91–180 days increased the risk by 30% (adjusted hazard ratio [aHR] 1.30, 95% CI 1.19–1.43) and delaying by over 180 days increased the risk by 94% (aHR 1.94, 95% CI 1.68–2.24). Five-year overall survival was 95.7% for 0–90 days, 93.0% for 91–180 days, and 87.9% for over 180 days. On subgroup analysis, increasing delay was associated with worse overall survival for T1, T2, and T3 tumors, but not T4 tumors.
Conclusions
Increasing time to surgery in papillary thyroid cancer is associated with reduced overall survival. Further research is necessary to assess the impact of surgical delay on disease-specific survival.


Similar content being viewed by others
References
Bott MJ, Patel AP, Crabtree TD, et al. Pathologic upstaging in patients undergoing resection for stage I non-small cell lung cancer: are there modifiable predictors? Ann Thorac Surg. 2015;100(6):2048–53.
Samson P, Patel A, Garrett T, et al. Effects of delayed surgical resection on short-term and long-term outcomes in clinical stage I non-small cell lung cancer. Ann Thorac Surg. 2015;99(6):1906–12 (discussion 1913).
Yang CJ, Wang H, Kumar A, et al. Impact of timing of lobectomy on survival for clinical stage IA lung squamous cell carcinoma. Chest. 2017;152(6):1239–50.
Kaltenmeier C, Shen C, Medich DS, et al. Time to surgery and colon cancer survival in the United States. Ann Surg. 2019. https://doi.org/10.1097/SLA.0000000000003745.
Grass F, Behm KT, Duchalais E, et al. Impact of delay to surgery on survival in stage I-III colon cancer. Eur J Surg Oncol. Mar ;46(3):455–61.
Polverini AC, Nelson RA, Marcinkowski E, et al. Time to treatment: measuring quality breast cancer care. Ann Surg Oncol. Oct ;23(10):3392–402.
Bleicher RJ, Ruth K, Sigurdson ER, et al. Time to surgery and breast cancer survival in the United States. JAMA Oncol. Mar ;2(3):330–9.
Patel KN, Yip L, Lubitz CC, et al. The American association of endocrine surgeons guidelines for the definitive surgical management of thyroid disease in adults. Ann Surg. Mar ;271(3):e21–93.
American College of Surgeons. National Cancer Database. Available at: https://www.facs.org/quality-programs/cancer/ncdb. Accessed 15 Jun 2020.
Haugen BR, Alexander EK, Bible KC, et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. Jan ;26(1):1–133.
Davies L, Welch HG. Thyroid cancer survival in the United States: observational data from 1973 to 2005. Arch Otolaryngol Head Neck Surg. 2010;136(5):440–4.
Shin DW, Cho J, Kim SY, et al. Delay to curative surgery greater than 12 weeks is associated with increased mortality in patients with colorectal and breast cancer but not lung or thyroid cancer. Ann Surg Oncol. 2013;20(8):2468–76.
Glockzin G, Hornung M, Kienle K, et al. Completion thyroidectomy: effect of timing on clinical complications and oncologic outcome in patients with differentiated thyroid cancer. World J Surg. 2012;36(5):1168–73.
Nam KH, Yoon JH, Chang HS, Park CS. Optimal timing of surgery in well-differentiated thyroid carcinoma detected during pregnancy. J Surg Oncol. 2005;91(3):199–203.
Uruno T, Shibuya H, Kitagawa W, Nagahama M, Sugino K, Ito K. Optimal timing of surgery for differentiated thyroid cancer in pregnant women. World J Surg. 2014;38(3):704–8.
Jeon MJ, Kim WG, Kwon H, et al. Clinical outcomes after delayed thyroid surgery in patients with papillary thyroid microcarcinoma. Eur J Endocrinol. 2017;177(1):25–31.
Ito Y, Miyauchi A, Inoue H, et al. An observational trial for papillary thyroid microcarcinoma in Japanese patients. World J Surg. 2010;34(1):28–35.
Mazzaferri EL, Jhiang SM. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med. Nov ;97(5):418–28.
Markt SC, Lago-Hernandez CA, Miller RE, et al. Insurance status and disparities in disease presentation, treatment, and outcomes for men with germ cell tumors. Cancer. 2016;122(20):3127–35.
Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in Self-reported insurance coverage, access to care, and health under the affordable care act. JAMA. Jul ;314(4):366–74.
Takvorian SU, Oganisian A, Mamtani R, et al. Association of medicaid expansion under the affordable care act with insurance status, cancer stage, and timely treatment among patients with breast, colon, and lung cancer. JAMA Netw Open. 2020;3(2):e1921653.
Naghavi AO, Echevarria MI, Grass GD, et al. Having medicaid insurance negatively impacts outcomes in patients with head and neck malignancies. Cancer. 2016;122(22):3529–37.
In H, Bilimoria KY, Stewart AK, et al. Cancer recurrence: an important but missing variable in national cancer registries. Ann Surg Oncol. 2014;21(5):1520–9.
James BC, Timsina L, Graham R, Angelos P, Haggstrom DA. Changes in total thyroidectomy versus thyroid lobectomy for papillary thyroid cancer during the past 15 years. Surgery. 2019;166(1):41–7.
Acknowledgment
The authors would like to thank Roger Davis, ScD, and Aaron Fleishman, MPH, for assistance with designing the biostatistical analysis.
Funding
This work was conducted with support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR002541) and financial contributions from Harvard University and its affiliated academic health care centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic health care centers, or the National Institutes of Health. Dr. Lubitz is also supported by the National Institutes of Health/National Cancer Institute Award R37 CA23195.
Author information
Authors and Affiliations
Contributions
Scott Fligor: Conceptualization, formal analysis, methodology, writing – original draft, writing – review and editing. Betzamel Lopez: Formal analysis, methodology, visualization, writing – original draft, writing – review and editing. Nishant Uppal: Methodology, writing – review and editing. Carrie Lubitz: Methodology, supervision, writing – review and editing. Benjamin James: Conceptualization, methodology, supervision, writing – review and editing.
Corresponding author
Ethics declarations
Disclosures
Scott C. Fligor, Betzamel Lopez, Nishant Uppal, Carrie C. Lubitz, and Benjamin C. James have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Scott C. Fligor and Betzamel Lopez are considered as co-first authors on this work.
Rights and permissions
About this article
Cite this article
Fligor, S.C., Lopez, B., Uppal, N. et al. Time to Surgery and Thyroid Cancer Survival in the United States. Ann Surg Oncol 28, 3556–3565 (2021). https://doi.org/10.1245/s10434-021-09797-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-09797-z