Abstract
Background
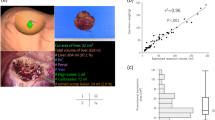
Hepatocellular carcinoma (HCC) is usually accompanied by different severities of cirrhosis, which is a risk factor for posthepatectomy liver failure (PHLF). Collagen proportional area (CPA) measurements can quantitatively determine the collagen contents of liver tissue. This study explored the impact of CPA on PHLF, and further investigated the correlation between CPA and a non-invasive method, namely cirrhotic severity scoring (CSS), previously proposed by our team.
Methods
A total of 224 HCC patients with Child–Pugh grade A liver function undergoing hepatectomy between 2017 and 2019 were retrospectively studied. Quantitative digital image analysis of resected liver tissues was used for the CPA measurement. Risk factors for PHLF were subjected to univariate and multivariate analyses, and the correlation between CPA and CSS was analyzed.
Results
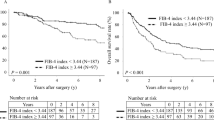
Overall, 28 (12.5%) patients experienced PHLF. Patients with PHLF had higher CPA values than those without PHLF (p < 0.001). Multivariate analysis showed CPA and extent of hepatectomy to be independent risk factors for PHLF. CPA values were divided into four stages based on their quartiles (C1: < 6.6%; C2: 6.6–10.7%; C3: 10.7–18.0%; C4: ≥ 18.0%). The incidence of PHLF increased with increasing CPA stages (p < 0.001). Furthermore, CSS was significantly correlated with CPA (r = 0.720; p < 0.001). The incidence of PHLF also increased with increasing severity of cirrhosis evaluated by CSS (p < 0.001).
Conclusions
In HCC patients with Child–Pugh grade A liver function, cirrhosis could be staged by liver collagen contents, which significantly influenced PHLF. Furthermore, CSS was useful in the preoperative evaluation of cirrhotic severity.





Similar content being viewed by others
References
El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557–76.
Akinyemiju T, Abera S, Ahmed M, et al. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: results from the global burden of disease study 2015. JAMA Oncol. 2017;3:1683–91.
Chen XP, Wu ZD, Huang ZY, Qiu FZ. Use of hepatectomy and splenectomy to treat hepatocellular carcinoma with cirrhotic hypersplenism. Br J Surg. 2005;92:334–9.
Dahiya D, Wu TJ, Lee CF, Chan KM, Lee WC, Chen MF. Minor versus major hepatic resection for small hepatocellular carcinoma (HCC) in cirrhotic patients: a 20-year experience. Surgery. 2010;147:676–85.
Zhou SJ, Zhang EL, Liang BY, et al. Morphologic severity of cirrhosis determines the extent of liver resection in patients with hepatocellular carcinoma and Child-Pugh grade A cirrhosis. J Surg Res. 2016;200:444–51.
Kim MY, Cho MY, Baik SK, et al. Histological subclassification of cirrhosis using the Laennec fibrosis scoring system correlates with clinical stage and grade of portal hypertension. J Hepatol. 2011;55:1004–9.
Standish RA, Cholongitas E, Dhillon A, Burroughs AK, Dhillon AP. An appraisal of the histopathological assessment of liver fibrosis. Gut. 2006;55:569–78.
Tsochatzis E, Bruno S, Isgro G, et al. Collagen proportionate area is superior to other histological methods for sub-classifying cirrhosis and determining prognosis. J Hepatol. 2014;60:948–54.
van Mierlo KM, Schaap FG, Dejong CH, Olde DS. Liver resection for cancer: new developments in prediction, prevention and management of postresectional liver failure. J Hepatol. 2016;65:1217–31.
Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149:713–24.
Zhang EL, Zhang ZY, Wang SP, et al. Predicting the severity of liver cirrhosis through clinical parameters. J Surg Res. 2016;204:274–81.
Jensen DM. Endoscopic screening for varices in cirrhosis: findings, implications, and outcomes. Gastroenterology. 2002;122:1620–30.
Pol B, Campan P, Hardwigsen J, Botti G, Pons J, Le Treut YP. Morbidity of major hepatic resections: a 100-case prospective study. Eur J Surg. 1999;165:446–53.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Dahab GM, Kheriza MM, El-Beltagi HM, Fouda AM, El-Din OA. Digital quantification of fibrosis in liver biopsy sections: description of a new method by Photoshop software. J Gastroenterol Hepatol. 2004;19:78–85.
Campos CF, Paiva DD, Perazzo H, et al. An inexpensive and worldwide available digital image analysis technique for histological fibrosis quantification in chronic hepatitis C. J Viral Hepat. 2014;21:216–22.
Zhang EL, Liang BY, Chen XP, Huang ZY. Severity of liver cirrhosis: a key role in the selection of surgical modality for Child–Pugh A hepatocellular carcinoma. World J Surg Oncol. 2015;13:148.
Calvaruso V, Burroughs AK, Standish R, et al. Computer-assisted image analysis of liver collagen: relationship to Ishak scoring and hepatic venous pressure gradient. Hepatology. 2009;49:1236–44.
Stasi C, Tsochatzis EA, Hall A, et al. Comparison and correlation of fibrosis stage assessment by collagen proportionate area (CPA) and the ELF panel in patients with chronic liver disease. Dig Liver Dis. 2019;51:1001–7.
Isgro G, Calvaruso V, Andreana L, et al. The relationship between transient elastography and histological collagen proportionate area for assessing fibrosis in chronic viral hepatitis. J Gastroenterol. 2013;48:921–9.
Fontana RJ, Goodman ZD, Dienstag JL, et al. Relationship of serum fibrosis markers with liver fibrosis stage and collagen content in patients with advanced chronic hepatitis C. Hepatology. 2008;47:789–98.
O’Brien MJ, Keating NM, Elderiny S, et al. An assessment of digital image analysis to measure fibrosis in liver biopsy specimens of patients with chronic hepatitis C. Am J Clin Pathol. 2000;114:712–8.
Manousou P, Dhillon AP, Isgro G, et al. Digital image analysis of liver collagen predicts clinical outcome of recurrent hepatitis C virus 1 year after liver transplantation. Liver Transpl. 2011;17:178–88.
Manousou P, Burroughs AK, Tsochatzis E, et al. Digital image analysis of collagen assessment of progression of fibrosis in recurrent HCV after liver transplantation. J Hepatol. 2013;58:962–8.
Huang Y, de Boer WB, Adams LA, MacQuillan G, Bulsara MK, Jeffrey GP. Image analysis of liver biopsy samples measures fibrosis and predicts clinical outcome. J Hepatol. 2014;61:22–7.
Siddique I, El-Naga HA, Madda JP, Memon A, Hasan F. Sampling variability on percutaneous liver biopsy in patients with chronic hepatitis C virus infection. Scand J Gastroenterol. 2003;38:427–32.
Regev A, Berho M, Jeffers LJ, et al. Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection. Am J Gastroenterol. 2002;97:2614–8.
Kawano Y, Sasaki A, Kai S, et al. Short- and long-term outcomes after hepatic resection for hepatocellular carcinoma with concomitant esophageal varices in patients with cirrhosis. Ann Surg Oncol. 2008;15:1670–6.
Mullen JT, Ribero D, Reddy SK, et al. Hepatic insufficiency and mortality in 1059 noncirrhotic patients undergoing major hepatectomy. J Am Coll Surg. 2007;204:854–62; discussion 862-4.
McCormack L, Petrowsky H, Jochum W, Furrer K, Clavien PA. Hepatic steatosis is a risk factor for postoperative complications after major hepatectomy: a matched case-control study. Ann Surg. 2007;245:923–30.
Farges O, Malassagne B, Flejou JF, Balzan S, Sauvanet A, Belghiti J. Risk of major liver resection in patients with underlying chronic liver disease: a reappraisal. Ann Surg. 1999;229:210–5.
Wang YY, Xiang BD, Ma L, et al. Development and validation of a nomogram to preoperatively estimate post-hepatectomy liver dysfunction risk and long-term survival in patients with hepatocellular carcinoma. Ann Surg. Epub 24 Feb 2020. https://doi.org/10.1097/sla.0000000000003803.
Wang YY, Zhong JH, Su ZY, et al. Albumin-bilirubin versus Child-Pugh score as a predictor of outcome after liver resection for hepatocellular carcinoma. Br J Surg. 2016;103:725–34.
Gu J, Zhang E, Liang B, Zhang Z, Chen X, Huang Z. Effectiveness comparison of indocyanine green retention test with the cirrhotic severity scoring in evaluating the pathological severity of liver cirrhosis in patients with hepatocellular carcinoma and Child-Pugh grade A liver function. World J Surg Oncol. 2020;18:79.
Acknowledgment
The authors thank Dr. Yaobing Chen and Dr. Cong Liu, Department of Pathology, Tongji Hospital, Huazhong University of Science and Technology, China, for their assistance in the pathological study.
Funding
This work was supported by funding from the National Science and Technology Major Project of China (No. 2017ZX10203207-002) to Prof. Zhiyong Huang, and funding from the National Natural Science Foundation of China (No. 81902839) to Dr. Erlei Zhang.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Jin Gu, Erlei Zhang, Binyong Liang, Zunyi Zhang, Xiaoping Chen, Min Xiong, and Zhiyong Huang declare they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gu, J., Zhang, E., Liang, B. et al. Liver Collagen Contents Are Closely Associated with the Severity of Cirrhosis and Posthepatectomy Liver Failure in Patients with Hepatocellular Carcinoma and Child–Pugh Grade A Liver Function. Ann Surg Oncol 28, 4227–4235 (2021). https://doi.org/10.1245/s10434-020-09557-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09557-5