Abstract
Introduction
Palliative chemotherapy (PC) is associated with a modest survival benefit in patients with incurable esophageal and gastric cancer; however, changes in symptom profile during treatment are not well described. Understanding the trajectory of symptoms during treatment may lead to improved care and facilitate shared decision making. In this study, we address this knowledge gap among all patients receiving PC in the Canadian province of Ontario.
Methods
Patients diagnosed with incurable esophageal and gastric cancer who received PC from 2012 to 2017 were identified from the Ontario Cancer Registry. Patients with one or more recorded Edmonton Symptom Assessment System (ESAS) scores in the 12 months following cancer diagnosis were included. The ESAS includes scores from 0 to 10 in nine domains (anxiety, depression, drowsiness, lack of appetite, nausea, pain, shortness of breath, tiredness, and lack of well-being). Symptom severity is categorized as none–mild (≤ 3), moderate (4–6), or severe (7–10). We focused on potentially modifiable symptoms, i.e. nausea, pain, and anxiety/depression. Logistic regression was used to identify factors associated with moderate–severe ESAS scores in these domains. Among those patients with serial ESAS scores (at 8 ± 2 and 12 ± 2 weeks) receiving chemotherapy, we describe changes during treatment (decrease by ≥ 1 = improved; − 1 > 0 > 1 = unchanged; increase by ≥ 1 = deteriorated).
Results
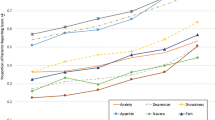
The cohort included 1900 patients who received PC, of whom 79% (1497/1900) had one or more recorded ESAS scores. In multivariate analysis, younger patients were more likely to have moderate–severe scores in nausea (odds ratio [OR] 1.89, 95% confidence interval [CI] 1.23–2.90 [p < 0.01] in patients aged 41–50 years compared with patients aged ≥ 71 years) and pain (OR 1.88, 95% CI 1.36–2.60 [p < 0.01] in patients aged 51–60 years compared with patients aged ≥ 71 years). Compared with males, females were more likely to report moderate–severe scores in anxiety/depression (OR 1.58, 95% CI 1.21–2.08 [p < 0.01]). At 8 ± 2 weeks from PC initiation, symptom scores were unchanged in 19–42% of patients, improved in 30–51% of patients, and deteriorated in 17–35% of patients. The greatest change in symptom burden was observed for appetite (51% improvement) and anxiety/depression (35% deterioration). Similar trends were observed at 12 ± 2 weeks.
Conclusions
In this large, population-based study, we observed that younger patients were more likely to report moderate–severe symptoms in pain and nausea, and females were more likely to report moderate–severe symptoms in anxiety/depression. Anxiety/depression symptoms become increasingly problematic for a substantial proportion of patients receiving PC. Supportive care efforts to mitigate these symptoms in routine practice are needed.


Similar content being viewed by others
References
Wagner AD, Syn NL, Moehler M, Grothe W, Yong WP, Tai BC, et al. Chemotherapy for advanced gastric cancer. Cochrane Database Syst Rev. 2017;8:CD004064.
Janmaat VT, Steyerberg EW, van der Gaast A, Mathijssen RH, Bruno MJ, Peppelenbosch MP, et al. Palliative chemotherapy and targeted therapies for esophageal and gastroesophageal junction cancer. Cochrane Database Syst Rev. 2017;11:CD004063.
Grunfeld EA, Maher EJ, Browne S, Ward P, Young T, Vivat B, et al. Advanced breast cancer patients’ perceptions of decision making for palliative chemotherapy. J Clin Oncol. 2006;24(7):1090–8.
Potgieter T, Maree JE. The palliative chemotherapy decision and experiences of South African patients and their families. Int J Palliat Nurs. 2018;24(6):272–80.
Merchant SJ, Brogly SB, Booth CM, Goldie C, Nanji S, Patel SV, et al. Palliative care and symptom burden in the last year of life: a population-based study of patients with gastrointestinal cancer. Ann Surg Oncol. 2019;26(8):2336–45.
Seow H, Barbera L, Sutradhar R, Howell D, Dudgeon D, Atzema C, et al. Trajectory of performance status and symptom scores for patients with cancer during the last six months of life. J Clin Oncol. 2011;29(9):1151–8.
Barbera L, Seow H, Howell D, Sutradhar R, Earle C, Liu Y, et al. Symptom burden and performance status in a population-based cohort of ambulatory cancer patients. Cancer 2010;116(24):5767–76.
Bubis LD, Davis L, Mahar A, Barbera L, Li Q, Moody L, et al. Symptom burden in the first year after cancer diagnosis: an analysis of patient-reported outcomes. J Clin Oncol. 2018;36(11):1103–11.
Wen FH, Chen JS, Chou WC, Hsieh CH, Chang WC, Shen WC, et al. Quality of life and psychological distress are differentially associated with distinct symptom-functional states in terminally ill cancer patients’ last year of life. Psychooncology 2018;27(9):2111–8.
Wilson KG, Chochinov HM, Skirko MG, Allard P, Chary S, Gagnon PR, et al. Depression and anxiety disorders in palliative cancer care. J Pain Symptom Manag. 2007;33(2):118–29.
Brooks GA, Abrams TA, Meyerhardt JA, Enzinger PC, Sommer K, Dalby CK, et al. Identification of potentially avoidable hospitalizations in patients with GI cancer. J Clin Oncol. 2014;32(6):496–503.
Barbera L, Atzema C, Sutradhar R, Seow H, Howell D, Husain A, et al. Do patient-reported symptoms predict emergency department visits in cancer patients? A population-based analysis. Ann Emerg Med. 2013;61(4):427–37.
Hui D, Bruera E. The edmonton symptom assessment system 25 years later: past, present, and future developments. J Pain Symptom Manag. 2017;53(3):630–43.
Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K. The edmonton symptom assessment system (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care. 1991;7(2):6–9.
Chang VT, Hwang SS, Feuerman M. Validation of the edmonton symptom assessment scale. Cancer 2000;88(9):2164–71.
Tran K, Zomer S, Chadder J, Earle C, Fung S, Liu J, et al. Measuring patient-reported outcomes to improve cancer care in Canada: an analysis of provincial survey data. Curr Oncol. 2018;25(2):176–9.
Moro C, Brunelli C, Miccinesi G, Fallai M, Morino P, Piazza M, et al. Edmonton symptom assessment scale: Italian validation in two palliative care settings. Support Care Cancer. 2006;14(1):30–7.
Shamieh O, Khamash O, Khraisat M, Jbouri O, Awni M, Al-Hawamdeh A, et al. Impact of outpatient palliative care (PC) on symptom burden in patients with advanced cancer at a tertiary cancer center in Jordan. Support Care Cancer. 2017;25(1):177–83.
Deodhar JK, Noronha V, Muckaden MA, Atreya S, Joshi A, Tandon SP, et al. A study to assess the feasibility of introducing early palliative care in ambulatory patients with advanced lung cancer. Indian J Palliat Care. 2017;23(3):261–7.
Pereira J, Green E, Molloy S, Dudgeon D, Howell D, Krzyzanowska MK, et al. Population-based standardized symptom screening: cancer care Ontario’s edmonton symptom assessment system and performance status initiatives. J Oncol Pract. 2014;10(3):212–4.
Li KK, Harris K, Hadi S, Chow E. What should be the optimal cut points for mild, moderate, and severe pain? J Palliat Med. 2007;10(6):1338–46.
Selby D, Cascella A, Gardiner K, Do R, Moravan V, Myers J, et al. A single set of numerical cutpoints to define moderate and severe symptoms for the edmonton symptom assessment system. J Pain Symptom Manag. 2010;39(2):241–9.
Robles SC, Marrett LD, Clarke EA, Risch HA. An application of capture-recapture methods to the estimation of completeness of cancer registration. J Clin Epidemiol. 1988;41(5):495–501.
Hui D, Shamieh O, Paiva CE, Perez-Cruz PE, Kwon JH, Muckaden MA, et al. Minimal clinically important differences in the edmonton symptom assessment scale in cancer patients: a prospective, multicenter study. Cancer 2015;121(17):3027–35.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;370(9596):1453–7.
Davis LE, Gupta V, Allen-Ayodabo C, Zhao H, Hallet J, Mahar AL, et al. Patient-reported symptoms following diagnosis in esophagus cancer patients treated with palliative intent. Dis Esophagus 2020;33(8):doz108.
Bodoky G, Scheulen ME, Rivera F, Jassem J, Carrato A, Moiseyenko V, et al. Clinical benefit and health-related quality of life assessment in patients treated with cisplatin/S-1 versus cisplatin/5-FU: secondary end point results from the first-line advanced gastric cancer study (FLAGS). J Gastrointest Cancer 2015;46(2):109–17.
Kripp M, Al-Batran SE, Rosowski J, Pauligk C, Homann N, Hartmann JT, et al. Quality of life of older adult patients receiving docetaxel-based chemotherapy triplets for esophagogastric adenocarcinoma: a randomized study of the Arbeitsgemeinschaft Internistische Onkologie (AIO). Gastric Cancer 2014;17(1):181–7.
van Kleef JJ, Ter Veer E, van den Boorn HG, Schokker S, Ngai LL, Prins MJ, et al. Quality of life during palliative systemic therapy for oesophagogastric cancer: systematic review and meta-analysis. J Natl Cancer Inst. 2020;112(1):12–29.
Woo A, Fu T, Popovic M, Chow E, Cella D, Wong CS, et al. Comparison of the EORTC STO-22 and the FACT-Ga quality of life questionnaires for patients with gastric cancer. Ann Palliat Med. 2016;5(1):13–21.
Cancer Care Ontario. Patient-Reported Outcomes and Symptom Management Program, Strategic Framework 2016–2019 [cited 6 May 2020]. https://www.cancercareontario.ca/sites/ccocancercare/files/assets/CCOPatientOutcomesStratFrame.pdf. Accessed 6 May 2020.
Weisman AD. Vulnerability and the psychological disturbances of cancer patients. Psychosomatics 1989;30(1):80–5.
Carlson LE, Tamagawa R, Stephen J, Drysdale E, Zhong L, Speca M. Randomized-controlled trial of mindfulness-based cancer recovery versus supportive expressive group therapy among distressed breast cancer survivors (MINDSET): long-term follow-up results. Psychooncology 2016;25(7):750–9.
Lengacher CA, Reich RR, Paterson CL, Ramesar S, Park JY, Alinat C, et al. Examination of broad symptom improvement resulting from mindfulness-based stress reduction in breast cancer survivors: a randomized controlled trial. J Clin Oncol. 2016;34(24):2827–34.
Rodin G, Lo C, Rydall A, Shnall J, Malfitano C, Chiu A, et al. Managing cancer and living meaningfully (CALM): a randomized controlled trial of a psychological intervention for patients with advanced cancer. J Clin Oncol. 2018;36(23):2422–32.
Cramer H, Lauche R, Klose P, Lange S, Langhorst J, Dobos GJ. Yoga for improving health-related quality of life, mental health and cancer-related symptoms in women diagnosed with breast cancer. Cochrane Database Syst Rev. 2017;1:CD010802.
Bekhet AH, Abdallah AR, Ismail HM, Genena DM, Osman NA, El Khatib A, et al. Benefits of aerobic exercise for breast cancer survivors: a systematic review of randomized controlled trials. Asian Pac J Cancer Prev. 2019;20(11):3197–209.
Nicholls SG, Langan SM, Benchimol EI. Routinely collected data: the importance of high-quality diagnostic coding to research. CMAJ. 2017;189(33):E1054–E5.
Funding
This study was funded by the CTAQ Endowment Fund, Queen’s University, awarded to Dr. Shaila Merchant.
Author information
Authors and Affiliations
Contributions
All authors contributed to (1) substantial contributions to the study conception and design, or analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content; (3) final approval of the version to be published; and (4) agreement to be accountable for all aspects of this work.
Corresponding author
Ethics declarations
Disclosure
Shaila J. Merchant, Weidong Kong, Michael Brundage, and Christopher M. Booth have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Merchant, S.J., Kong, W., Brundage, M. et al. Symptom Evolution in Patients with Esophageal and Gastric Cancer Receiving Palliative Chemotherapy: A Population-Based Study. Ann Surg Oncol 28, 79–87 (2021). https://doi.org/10.1245/s10434-020-09289-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09289-6