Abstract
Background
The impact of the number of examined lymph nodes (ELNs) on stage correction and prognostication in patients with esophageal squamous cell carcinoma (ESCC) who underwent right transthoracic esophagectomy is still unclear.
Methods
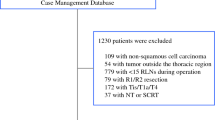
Patients with ESCC who underwent right transthoracic esophagectomy at Sun Yat-sen University Cancer Center between January 1997 and December 2013 were retrospectively enrolled. The Cox proportional hazards regression model was used to determine the effect of ELN count on overall survival. The impact of ELN count on stage correction was evaluated using the hypergeometric distribution and Bayes theorem and β-binomial distribution estimation, respectively. The threshold of ELNs was determined using the LOWESS smoother and piecewise linear regression.
Results
Among the 875 included patients, greater ELNs were associated with a higher rate of nodal metastasis. Significant association between staging bias and the number of ELNs is only observed through the Bayes method. The ELN count did not impact 90-day mortality but significantly impacted long-term survival (adjusted hazard ratio [aHR] 0.986), especially in those patients with node-negative disease (aHR 0.972). In patients with node-negative disease, cut-point analysis showed a threshold ELN count of 21.
Conclusions
A greater number of ELNs is associated with more accurate node staging and better long-term survival in resected ESCC patients. We recommended harvesting at least 21 LNs to acquire accurate staging and long-term survival information for patients with declared node-negative disease using the right thoracic approach.


Similar content being viewed by others
References
Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–32.
Veeramachaneni NK, Zoole JB, Decker PA, et al. Lymph node analysis in esophageal resection: American College of Surgeons Oncology Group Z0060 trial. Ann Thorac Surg. 2008;86:418–21; discussion 21.
Herskovic A, Russell W, Liptay M, Fidler MJ, Al-Sarraf M. Esophageal carcinoma advances in treatment results for locally advanced disease: review. Ann Oncol. 2012;23: 1095–103.
Yang D, Mao YS, He J, et al. Long-term survival of the middle and lower thoracic esophageal cancer patients after surgical treatment through left or right thoracic approach. J Thorac Dis. 2018;10: 2648–55.
Li B, Xiang J, Zhang Y, et al. Comparison of Ivor-Lewis vs Sweet esophagectomy for esophageal squamous cell carcinoma: a randomized clinical trial. JAMA Surg. 2015;150: 292–8.
Li B, Hu H, Zhang Y, et al. Extended Right Thoracic Approach Compared With Limited Left Thoracic Approach for Patients With Middle and Lower Esophageal Squamous Cell Carcinoma: Three-year Survival of a Prospective, Randomized, Open-label Trial. Ann Surg. 2018;267: 826–32.
Zheng YZ, Zhao W, Hu Y, et al. Aggressive surgical resection does not improve survival in operable esophageal squamous cell carcinoma with N2-3 status. World J Gastroenterol. 2015;21: 8644–52.
Yang HX, Xu Y, Fu JH, et al. An evaluation of the number of lymph nodes examined and survival for node-negative esophageal carcinoma: data from China. Ann Surg Oncol. 2010;17: 1901–11.
van der Werf LR, Dikken JL, van Berge Henegouwen MI, et al. A Population-based Study on Lymph Node Retrieval in Patients with Esophageal Cancer: Results from the Dutch Upper Gastrointestinal Cancer Audit. Ann Surg Oncol. 2018;25: 1211–20.
Bogoevski D, Onken F, Koenig A, et al. Is it time for a new TNM classification in esophageal carcinoma? Ann Surg. 2008;247: 633–41.
Bollschweiler E, Baldus SE, Schroder W, Schneider PM and Holscher AH. Staging of esophageal carcinoma: length of tumor and number of involved regional lymph nodes. Are these independent prognostic factors? J Surg Oncol. 2006;94: 355–63.
National Comprehensive Cancer Network. Esophageal and Esophagogastric Junction Cancers. Version 1.2019. Available at: https://www.nccn.org/professionals/physician_gls/pdf/esophageal.pdf.
Rice TW, Chen LQ, Hofstetter WL, et al. Worldwide Esophageal Cancer Collaboration: pathologic staging data. Dis Esophagus. 2016;29: 724–33.
Giugliano DN, Berger AC, Pucci MJ, et al. Comparative Quantitative Lymph Node Assessment in Localized Esophageal Cancer Patients After R0 Resection With and Without Neoadjuvant Chemoradiation Therapy. J Gastrointest Surg. 2017;21: 1377–84.
He J. Thoracic oncology. Beijing: People’s Medical Publishing House; 2013.
Tan Z, Ma G, Yang H, et al. Can lymph node ratio replace pn categories in the tumor-node-metastasis classification system for esophageal cancer? J Thorac Oncol. 2014;9: 1214–21.
Yildiz MM, Petersen I, Eigendorff E, Schlattmann P and Guntinas-Lichius O. Which is the most suitable lymph node predictor for overall survival after primary surgery of head and neck cancer: pN, the number or the ratio of positive lymph nodes, or log odds? J Cancer Res Clin Oncol. 2016;142: 885–93.
Zhan C, Shi Y, Jiang W, et al. How many lymph nodes should be dissected in esophagectomy with or without neoadjuvant therapy to get accurate staging? Dis Esophagus. 2020;33(1):doz009.
Kiricuta CI, Tausch J. A mathematical model of axillary lymph node involvement based on 1446 complete axillary dissections in patients with breast carcinoma. Cancer. 1992;69: 2496–501.
Gonen M, Schrag D, Weiser MR. Nodal staging score: a tool to assess adequate staging of node-negative colon cancer. J Clin Oncol. 2009;27: 6166–71.
Greenstein AJ, Litle VR, Swanson SJ, et al. Effect of the number of lymph nodes sampled on postoperative survival of lymph node-negative esophageal cancer. Cancer. 2008;112: 1239–46.
Wang J, Wei N, Jiang N, Lu Y, Zhang X. Comparison of Ivor-Lewis versus Sweet procedure for middle and lower thoracic esophageal squamous cell carcinoma: A STROBE compliant study. Medicine (Baltimore). 2019;98: e14416.
Zhang SS, Yang H, Xie X, et al. Adjuvant chemotherapy versus surgery alone for esophageal squamous cell carcinoma: a meta-analysis of randomized controlled trials and nonrandomized studies. Dis Esophagus. 2014;27: 574–84.
Yu S, Zhang W, Ni W, et al. A propensity-score matching analysis comparing long-term survival of surgery alone and postoperative treatment for patients in node positive or stage III esophageal squamous cell carcinoma after R0 esophagectomy. Radiother Oncol. 2019;140: 159–66.
Faiz Z, Lemmens VE, Siersema PD, et al. Increased resection rates and survival among patients aged 75 years and older with esophageal cancer: a Dutch nationwide population-based study. World J Surg. 2012;36: 2872–8.
Ruol A, Castoro C, Portale G, et al. Trends in management and prognosis for esophageal cancer surgery: twenty-five years of experience at a single institution. Arch Surg. 2009;144: 247–54; discussion 54.
Acknowledgments
This study was supported by the Medical Scientific Research Foundation of Guangdong Province of China (Grant No. A2020150), Natural Science Foundation of Guangdong Province of China (Grant Nos. 2017A030310641, 2018A030313762), and Medical Scientific Research Foundation of Guangdong Province of China (Grant No. A2018301).
Funding
The funding source had no role in the design of this study and did not have any role during its execution, analyses, interpretation of the data, or decision to submit the results.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Fig. S1
Distribution of the number of harvested lymph nodes (TIFF 92 kb)
Supplementary Fig. S2
Probability of false stage and confidence of accurate nodal stage when a different number of LNs is examined in patients with N0, N1, and N2 status (TIFF 1507 kb)
Supplementary Fig. S3
Overall survival stratified by examined lymph node (ELN) count of 21 for the entire, N−, and N+ cohorts (TIFF 885 kb)
Rights and permissions
About this article
Cite this article
Zheng, YZ., Li, XQ., Wang, JY. et al. Impact of Examined Lymph Node Count for Esophageal Squamous Cell Carcinoma in Patients who Underwent Right Transthoracic Esophagectomy. Ann Surg Oncol 28, 3025–3033 (2021). https://doi.org/10.1245/s10434-020-09217-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09217-8