Abstract
Background
This study aimed to evaluate the impact of rapid genetic testing (RGT) for BRCA1 and BRCA2 at the time of breast cancer diagnosis on treatment choices. Bilateral mastectomy for the treatment of breast cancer in women with a BRCA1 or BRCA2 mutation offers a reduction in the risk of contralateral breast cancer. It is unclear whether offering RGT at the time of breast cancer diagnosis has an impact on women’s surgical decision-making.
Methods
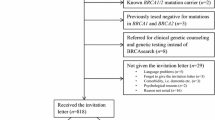
Women with breast cancer diagnosed between June 2013 and May 2018 were recruited from four academic health sciences centers in Toronto, Canada. The participants completed a questionnaire before genetic testing, then one week and one year after disclosure of the genetic test result. Before surgery, RGT was performed. Diagnostic, pathologic, and treatment data were compared between those with and those without a BRCA mutation.
Results
The study enrolled 1007 women who consented to RGT. The mean age of the participants was 46.3 years, and the median time to result disclosure was 10 days. A BRCA mutation was found in 6% of the women. The women with a BRCA mutation were significantly more likely to elect for bilateral mastectomy than the women without a BRCA mutation (p < 0.0001). Of the BRCA-positive patients, 95.7% reported that they used their genetic test result to make a surgical decision.
Conclusions
The women provided with RGT at the time of breast cancer diagnosis use the genetic information to make treatment decisions, and the majority of those identified with a BRCA mutation elect for a bilateral mastectomy.
Similar content being viewed by others
References
Metcalfe K, Gershman S, Ghadirian P, et al. Contralateral mastectomy and survival after breast cancer in carriers of BRCA1 and BRCA2 mutations: retrospective analysis. BMJ. 2014;348:g226.
Metcalfe K, Lynch HT, Foulkes WD, et al. Effect of oophorectomy on survival after breast cancer in BRCA1 and BRCA2 mutation carriers. JAMA Oncol. 2015;1:306–13.
Finch AP, Lubinski J, Moller P, et al. Impact of oophorectomy on cancer incidence and mortality in women with a BRCA1 or BRCA2 mutation. J Clin Oncol. 2014;32:1547.
Beitsch PD, Whitworth PW, Hughes K, et al. Underdiagnosis of hereditary breast cancer: are genetic testing guidelines a tool or an obstacle? J Clin Oncol. 2019;37:453–60.
Rajagopal PS, Catenacci DVT, Olopade OI. The time for mainstreaming germline testing for patients with breast cancer is now. J Clin Oncol. 2019;37:2177–8.
Copur MS, Jonglertham P, Zusag T. Should all patients with a diagnosis of breast cancer undergo expanded panel testing? J Clin Oncol. 2019;37:2175–6.
Milliron KJ, Griggs JJ. Advances in genetic testing in patients with breast cancer, high-quality decision making, and responsible resource allocation. J Clin Oncol. 2019;37:445–7.
Manahan ER, Kuerer HM, Sebastian M, et al. Consensus guidelines on genetic testing for hereditary breast cancer from the American Society of Breast Surgeons. Ann Surg Oncol. 2019;26:3025–31.
Force UPST. Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer: U.S. Preventive Services Task Force Recommendation Statement. JAMA. 2019;322:652–65.
Pal T, Agnese D, Daly M, et al. Points to consider: is there evidence to support BRCA1/2 and other inherited breast cancer genetic testing for all breast cancer patients? A statement of the American College of Medical Genetics and Genomics (ACMG). Genet Med. 2019;22:681–5.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Genetic/Familial High-Risk Assessment: Breast and Ovarian. 2019.
Metcalfe K, Gershman S, Lynch HT, et al. Predictors of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. Br J Cancer. 2011;104:1384–92.
Metcalfe K, Lynch HT, Ghadirian P, et al. Contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2004;22:2328–35.
Metcalfe KA, Lubinski J, Ghadirian P, et al. Predictors of contralateral prophylactic mastectomy in women with a BRCA1 or BRCA2 mutation: the Hereditary Breast Cancer Clinical Study Group. J Clin Oncol. 2008;26:1093–7.
Schwartz MD, Peshkin BN, Isaacs C, et al. Randomized trial of proactive rapid genetic counseling versus usual care for newly diagnosed breast cancer patients. Breast Cancer Res Treat. 2018;170:517–24.
Wevers MR, Aaronson NK, Verhoef S, et al. Impact of rapid genetic counselling and testing on the decision to undergo immediate or delayed prophylactic mastectomy in newly diagnosed breast cancer patients: findings from a randomised controlled trial. Br J Cancer. 2014;110:1081–7.
Huzarski T, Byrski T, Gronwald J, et al. The impact of oophorectomy on survival after breast cancer in BRCA1-positive breast cancer patients. Breast Cancer Res Treat. 2016;156:371–8.
Narod SA, Huzarski T, Gronwald J, et al. Predictors of survival for breast cancer patients with a BRCA1 mutation. Breast Cancer Res Treat. 2018;168:513–21.
Metcalfe K, Eisen A, Senter L, et al. International trends in the uptake of cancer risk reduction strategies in women with a BRCA1 or BRCA2 mutation. Br J Cancer. 2019;121:15–21.
Metcalfe K, Lynch HT, Foulkes WD, et al. Oestrogen receptor status and survival in women with BRCA2-associated breast cancer. Br J Cancer. 2019;120:398–403.
Jonasson JG, Stefansson OA, Johannsson OT, et al. Oestrogen receptor status, treatment, and breast cancer prognosis in Icelandic BRCA2 mutation carriers. Br J Cancer. 2016;115:776–83.
Funding
This study was funded by a Canadian Institutes of Health Research (CIHR) Grant awarded to Kelly A. Metcalfe.
Author information
Authors and Affiliations
Contributions
KM conceived the study. PS was responsible for the statistical analysis. SN and KM drafted the manuscript. All authors were involved in participant enrollment and data collection. All authors reviewed the final manuscript.
Corresponding author
Ethics declarations
Disclosures
Jenna McCuaig received speaker honoraria from AstraZeneca Canada and Pfizer Canada. The remaining authors have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Metcalfe, K.A., Eisen, A., Poll, A. et al. Rapid Genetic Testing for BRCA1 and BRCA2 Mutations at the Time of Breast Cancer Diagnosis: An Observational Study. Ann Surg Oncol 28, 2219–2226 (2021). https://doi.org/10.1245/s10434-020-09160-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09160-8