Abstract
Background
Although bile duct resection (BDR) in addition to pancreaticoduodenectomy (PD) is considered a surgical approach in patients with middle-third cholangiocarcinoma (MCC), available prognostic information after BDR remains very limited. The aim of this study was to reappraise BDR from the viewpoint of surgical oncology.
Methods
Patients who underwent BDR or PD for MCC between 2001 and 2010 at 32 Japanese hospitals were included. Clinicopathological factors were retrospectively compared according to surgical procedure to identify a subset cohort who benefited most from BDR.
Results
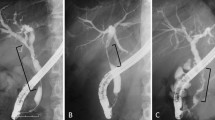
During the study, 92 patients underwent BDR (n = 38) or PD (n = 54). BDR was characterized by a shorter operation time, less blood loss, less frequent complications, and lower mortality, than PD. The incidence of positive surgical margins was 26.3% versus 5.6% (P = 0.007). The survival rate after BDR was significantly worse than that after PD: 38.8% versus 54.8% at 5 years (P = 0.035), and BDR was independently associated with deteriorated survival [hazard ratio (HR), 1.76; P = 0.023] by multivariable analysis. In the BDR group, tumor length < 15 mm (HR, 3.38; P = 0.017) and ductal margin length ≥ 10 mm (HR, 2.54; P = 0.018) were independent positive prognostic factors. Stratified by these two favorable factors, the 5-year survival rate was 63.0% in patients with 1/2 factors and 6.7% in those with 0 factors (P < 0.001).
Conclusion
In patients with MCC, BDR provided a better short-term and a worse long-term outcome than PD. However, patient selection using tumor length and ductal margin length may allow a favorable survival probability even after BDR.


Similar content being viewed by others
References
Nakeeb A, Pitt HA, Sohn TA, et al. Cholangiocarcinoma: a spectrum of intrahepatic, perihilar, and distal tumors. Ann Surg. 1996;224(4):463–73.
Kiriyama M, Ebata T, Aoba T, et al. Prognostic impact of lymph node metastasis in distal cholangiocarcinoma. Br J Surg. 2015;102(4):399–406.
Komaya K, Ebata T, Fukami Y, et al. Percutaneous biliary drainage is oncologically inferior to endoscopic drainage: a propensity score matching analysis in resectable distal cholangiocarcinoma. J Gastroenterol. 2016;51(6):608–19.
Maeta T, Ebata T, Hayashi E, et al. Pancreatoduodenectomy with portal vein resection for distal cholangiocarcinoma. Br J Surg. 2017;104(11):1549–57.
Reding R, Buard JL, Lebeau G, Launois B. Surgical management of 552 carcinomas of the extrahepatic bile ducts (gallbladder and periampullary tumors excluded). Results of the French Surgical Association Survey. Ann Surg. 1991;213(3):236–41.
Carroll JE, Jr., Hurwitz ZM, Simons JP, et al. In-hospital mortality after resection of biliary tract cancer in the United States. HPB (Oxford). 2010;12(1):62–7.
Strijker M, Belkouz A, van der Geest LG, et al. Treatment and survival of resected and unresected distal cholangiocarcinoma: a nationwide study. Acta Oncol. 2019;58(7):1048–55.
Kwon HJ, Kim SG, Chun JM, Lee WK, Hwang YJ. Prognostic factors in patients with middle and distal bile duct cancers. World J Gastroenterol. 2014;20(21):6658–65.
Kim N, Lee H, Min SK, Lee HK. Bile duct segmental resection versus pancreatoduodenectomy for middle and distal common bile duct cancer. Ann Surg Treat Res. 2018;94(5):240–46.
Schreuder AM, Engelsman AF, van Roessel S, et al. Treatment of mid-bile duct carcinoma: local resection or pancreatoduodenectomy? Eur J Surg Oncol. 2019;45(11):2180–87.
Kayahara M, Nagakawa T, Ohta T, Kitagawa H, Tajima H, Miwa K. Role of nodal involvement and the periductal soft-tissue margin in middle and distal bile duct cancer. Ann Surg. 1999;229(1):76–83.
Fong Y, Blumgart LH, Lin E, Fortner JG, Brennan MF. Outcome of treatment for distal bile duct cancer. Br J Surg. 1996;83(12):1712–15.
Jang JY, Kim SW, Park DJ, et al. Actual long-term outcome of extrahepatic bile duct cancer after surgical resection. Ann Surg. 2005;241(1):77–84.
Ikeyama T, Nagino M, Oda K, Ebata T, Nishio H, Nimura Y. Surgical approach to bismuth Type I and II hilar cholangiocarcinomas: audit of 54 consecutive cases. Ann Surg. 2007;246(6):1052–57.
Ebata T, Watanabe H, Ajioka Y, Oda K, Nimura Y. Pathological appraisal of lines of resection for bile duct carcinoma. Br J Surg. 2002;89(10):1260–7.
Japanese Society of Biliary Surgery. Classification of Biliary Tract Carcinoma, 2nd English ed. Tokyo: Kanehara; 2004.
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, eds. AJCC Cancer Staging Manual. 7th ed. New York: Springer; 2010.
Wakai T, Shirai Y, Moroda T, Yokoyama N, Hatakeyama K. Impact of ductal resection margin status on long-term survival in patients undergoing resection for extrahepatic cholangiocarcinoma. Cancer. 2005;103(6):1210–16.
Igami T, Nagino M, Oda K, et al. Clinicopathologic study of cholangiocarcinoma with superficial spread. Ann Surg. 2009;249(2):296–302.
Ebata T, Yokoyama Y, Igami T, et al. Hepatopancreatoduodenectomy for cholangiocarcinoma: a single-center review of 85 consecutive patients. Ann Surg. 2012;256(2):297–305.
Kawai M, Kondo S, Yamaue H, et al. Predictive risk factors for clinically relevant pancreatic fistula analyzed in 1239 patients with pancreaticoduodenectomy: multicenter data collection as a project study of pancreatic surgery by the Japanese Society of Hepato-Biliary-Pancreatic Surgery. J Hepatobiliary Pancreat Sci. 2011;18(4):601–8.
Kimura W, Miyata H, Gotoh M, et al. A pancreaticoduodenectomy risk model derived from 8575 cases from a national single-race population (Japanese) using a web-based data entry system: the 30-day and in-hospital mortality rates for pancreaticoduodenectomy. Ann Surg. 2014;259(4):773–80.
Schwarz RE, Smith DD. Lymph node dissection impact on staging and survival of extrahepatic cholangiocarcinomas, based on U.S. population data. J Gastrointest Surg. 2007;11(2):158–65.
Bhuiya MR, Nimura Y, Kamiya J, et al. Clinicopathologic studies on perineural invasion of bile duct carcinoma. Ann Surg. 1992;215(4):344–9.
Otsuka S, Ebata T, Yokoyama Y, et al. Clinical value of additional resection of a margin-positive distal bile duct in perihilar cholangiocarcinoma. Br J Surg. 2019;106(6):774–82.
Komaya K, Ebata T, Shirai K, et al. Recurrence after resection with curative intent for distal cholangiocarcinoma. Br J Surg. 2017;104(4):426–33.
Komaya K, Ebata T, Yokoyama Y, et al. Recurrence after curative-intent resection of perihilar cholangiocarcinoma: analysis of a large cohort with a close postoperative follow-up approach. Surgery. 2018;163(4):732–8.
Hwang S, Lee SG, Kim KH, et al. Extended extrahepatic bile duct resection to avoid performing pancreatoduodenectomy in patients with mid bile duct cancer. Dig Surg. 2008;25(1):74–9.
Lee HG, Lee SH, Yoo DD, et al. Carcinoma of the middle bile duct: is bile duct segmental resection appropriate? World J Gastroenterol. 2009;15(47):5966–71.
Lee HY, Kim SH, Lee JM, et al. Preoperative assessment of resectability of hepatic hilar cholangiocarcinoma: combined CT and cholangiography with revised criteria. Radiology. Apr 2006;239(1):113–21.
Ni Q, Wang H, Zhang Y, et al. MDCT assessment of resectability in hilar cholangiocarcinoma. Abdom Radiol (NY). 2017;42(3):851–60.
Acknowledgements
The authors are grateful to the following investigators in the Nagoya Surgical Oncology Group: T. Aoba (Toyohashi Municipal Hospital, Toyohashi), Y. Kaneoka (Ogaki Municipal Hospital, Ogaki), T. Arai (Anjo Kosei Hospital, Anjo), Y. Shimizu (Aichi Cancer Center Hospital, Nagoya), G. Sugawara (Toyota Kosei Hospital, Toyota), H. Miyake (Japanese Red Cross Nagoya Daiichi Hospital, Nagoya), E. Sakamoto (Japanese Red Cross Nagoya Daini Hospital, Nagoya), K. Shirai (Yamashita Hospital, Ichinomiya), Y. Okada (Handa City Hospital, Handa), E. Hayashi (Japan Community Health care Organization Chukyo Hospital, Nagoya), Y. Kato (Nagoya Ekisaikai Hospital, Nagoya), R. Yamaguchi (Kasugai Municipal Hospital, Kasugai), S. Kobayashi (Kumiai Kosei Hospital, Takayama), Y. Uno (Daido Hospital, Nagoya), T. Maeta (JA Shizuoka Kohseiren Enshu Hospital, Hamamatsu), S. Mizuno (Shizuoka Welfare Hospital, Shizuoka), H. Yamamoto (Tokai Hospital, Nagoya), K. Akashi (Hekinan Municipal Hospital, Hekinan), M. Takano (Asahi Rousai Hospital, Owariasahi), M. Uno (Tokoname City Hospital, Tokoname), and M. Hattori (Nishichita General Hospital, Chita).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosure
The authors declare no conflicts of interest associated with this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jikei, K., Ebata, T., Mizuno, T. et al. Oncologic Reappraisal of Bile Duct Resection for Middle-Third Cholangiocarcinoma. Ann Surg Oncol 28, 1990–1999 (2021). https://doi.org/10.1245/s10434-020-09157-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09157-3