Abstract
Introduction
With limited data in regards to management, occult breast cancer (OBC) poses a challenging surgical scenario. Current surgical management includes axillary lymphadenectomy (ALND) with or without mastectomy. We sought to investigate the impact of hospital volume on surgical approach and survival outcomes of patients with OBC.
Methods
Patients with cT0N+ breast cancer were selected from the National Cancer Data Base (NCDB, 2004–2014). Primary outcome was overall survival (OS), calculated using Kaplan–Meier methods compared according to hospital volume: community cancer center (CC), comprehensive community cancer center (COMP), and academic center (AC). Secondary outcome was the rate of modified radical mastectomy (MRM).
Results
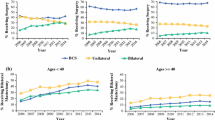
We identified 574 patients with OBC, 11.1% were treated at a CC, 51.8% at a COMP, and 37.0% at an AC. Patients treated at CC had lower socioeconomic status compared with COMP or AC (23.1%, 14.1%, 19.3%; p = 0.005, respectively). There was no difference in access to radiation therapy (p = 0.888) or neoadjuvant chemotherapy (p = 0.221). Patients treated at CC had worse OS compared with COMP or AC (87.04, 105.29, 108.06 mo, p = 0.026, respectively). There was an increased rate of MRM at CC compared with COMP or AC (54.7%, 41.2%, 30.5%, p = 0.003, respectively).
Conclusions
A direct association seems to exist between hospital volume and outcomes of patients with OBC. Patients with OBC treated at AC were more likely to undergo breast-conserving approaches and had better survival than those treated at CC.



Similar content being viewed by others
References
Baron PL, Moore MP, Kinne DW, Candela FC, Osborne MP, Petrek JA. Occult breast cancer presenting with axillary metastases: updated management. Arch Surg. 1990;125(2):210–4.
Vlastos G, Jean ME, Mirza AN, et al. Feasibility of breast preservation in the treatment of occult primary carcinoma presenting with axillary metastases. Ann Surg Oncol. 2001;8(5):425–31.
Ge L-P, Liu X-Y, Xiao Y, et al. Clinicopathological characteristics and treatment outcomes of occult breast cancer: a SEER population-based study. Cancer Manage Res. 2018;10:4381.
Macedo FI, Eid JJ, Flynn J, Jacobs MJ, Mittal VK. Optimal surgical management for occult breast carcinoma: a meta-analysis. Ann Surg Oncol. 2016;23(6):1838–44.
Network NCC. NCCN guidelines version 1. Invasive breast cancer. 2018.
Guller U, Safford S, Pietrobon R, Heberer M, Oertli D, Jain NB. High hospital volume is associated with better outcomes for breast cancer surgery: analysis of 233,247 patients. World J Surg. 2005;29(8):994–9.
Finlayson EV, Goodney PP, Birkmeyer JD. Hospital volume and operative mortality in cancer surgery: a national study. Arch Surg. 2003;138(7):721–5.
Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137(6):511–20.
Davoli M, Amato L, Minozzi S, Bargagli A, Vecchi S, Perucci C. Volume and health outcomes: an overview of systematic reviews. 2005.
Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128–37.
Chen C-S, Liu T-C, Lin H-C, Lien Y-C. Does high surgeon and hospital surgical volume raise the five-year survival rate for breast cancer? A population-based study. Breast Cancer Res Treat. 2008;110(2):349–56.
Yen TW, Pezzin LE, Li J, Sparapani R, Laud PW, Nattinger AB. Effect of hospital volume on processes of breast cancer care: a National Cancer Data Base study. Cancer. 2017;123(6):957–66.
Vrijens F, Stordeur S, Beirens K, Devriese S, Van Eycken E, Vlayen J. Effect of hospital volume on processes of care and 5-year survival after breast cancer: a population-based study on 25,000 women. Breast. 2012;21(3):261–6.
Kong AL, Pezzin LE, Nattinger AB. Identifying patterns of breast cancer care provided at high-volume hospitals: a classification and regression tree analysis. Breast Cancer Res Treat. 2015;153(3):689–98.
Cancer ACoSCo. Cancer program standards: ensuring patient-centered care. facs.org/~/media/files/quality%20programs/cancer/coc/2016%20coc%20standards%20manual_interactive%20pdf.ashx. 2016.
Greenup RA, Obeng-Gyasi S, Thomas S, et al. The effect of hospital volume on breast cancer mortality. Ann Surg. 2018;267(2):375.
Gutierrez JC, Hurley JD, Housri N, et al. Are many community hospitals undertreating breast cancer? Lessons from 24,834 patients. Ann Surg. 2008;248(2):154–62.
Bilimoria KY, Bentrem DJ, Stewart AK, Winchester DP, Ko CY. Comparison of Commission on Cancer–approved and–nonapproved hospitals in the United States: implications for studies that use the National Cancer Data Base. J Clin Oncol. 2009;27(25):4177–81.
Cohen BL, Collier AL, Kelly KN, et al. Surgical management of the axilla in patients with occult breast cancer (cT0 N+) after neoadjuvant chemotherapy. Ann Surg Oncol. 2020:1–12.
Corradini S, Reitz D, Pazos M, et al. Mastectomy or breast-conserving therapy for early breast cancer in real-life clinical practice: outcome comparison of 7565 cases. Cancers. 2019;11(2):160.
Hessler LK, Molitoris JK, Rosenblatt PY, et al. Factors influencing management and outcome in patients with occult breast cancer with axillary lymph node involvement: analysis of the National Cancer Database. Ann Surg Oncol. 2017;24(10):2907–14.
Gooiker G, Van Gijn W, Wouters M, et al. Systematic review and meta-analysis of the volume–outcome relationship in pancreatic surgery. Br J Surg. 2011;98(4):485–94.
Pezzin LE, Laud P, Yen T, Neuner J, Nattinger AB. Re-examining the relationship of breast cancer hospital and surgical volume to mortality: an instrumental variable analysis. Med Care. 2015;53(12):1033.
Funding
None declared.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Baumrucker, C.C., Spring, S.R., Cohen, B.L. et al. The Effect of Hospital Volume on Outcomes of Patients with Occult Breast Cancer. Ann Surg Oncol 28, 2128–2135 (2021). https://doi.org/10.1245/s10434-020-09103-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09103-3