Abstract
Background
The prediction of prognostic outcomes can provide the most suitable strategy for patients with pancreatic ductal adenocarcinoma (PDAC). This study aimed to evaluate the clinical value of the preoperative tumor marker index (pre-TI) in predicting prognostic outcomes after resection for PDAC.
Methods
For 183 patients who underwent pancreatic resection of PDAC, adjusted carbohydrate antigen 19-9 (CA19-9), carcinoembryonic antigen (CEA), pancreatic cancer-associated antigen-2 (DUpan-2), and s-pancreas-1 antigen (SPan-1) were retrospectively evaluated, and the positive number of these markers was scored as the pre-TI.
Results
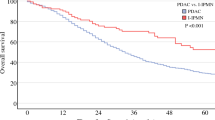
A high pre-TI (≥ 2) was significantly associated with a larger tumor and lymph node metastases, and the patients with a high pre-TI had worse prognostic outcomes in terms of both relapse-free survival (RFS) (P < 0.0001, log-rank) and overall survival (OS) (P < 0.0001, Λlog-rank) than the patients with a low pre-TI. The pre-TI was one of the independent factors of a poor prognosis for RFS (hazard ratio [HR], 2.36; P < 0.0001) and OS (HR, 2.27; P < 0.0001). In addition, even for the patients with normal adjusted CA19-9 values (n = 74, 40.4%), those with the high pre-TI had a significantly poorer prognosis than those with a low pre-TI (RFS: P = 0.002, log-rank; OS: P = 0.031, log-rank).
Conclusions
The pre-TI could be a potent predictive marker of prognostic outcomes for patients with resections for PDAC. Patients with a high pre-TI may need additional strategies to improve their prognosis.



Similar content being viewed by others
References
Ryan DP, Hong TS, Bardeesy N. Pancreatic adenocarcinoma. N Engl J Med. 2014;371:1039–49.
Uesaka K, Boku N, Fukutomi A, et al. Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: a phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet. 2016;388:248–57.
Cloyd JM, Wang H, Egger ME, et al. Association of clinical factors with a major pathologic response following preoperative therapy for pancreatic ductal adenocarcinoma. JAMA Surg. 2017;152:1048–56.
Mokdad AA, Minter RM, Zhu H, et al. Neoadjuvant therapy followed by resection versus upfront resection for resectable pancreatic cancer: a propensity score-matched analysis. J Clin Oncol. 2017;35:515–22.
Maggino L, Malleo G, Marchegiani G, et al. Outcomes of primary chemotherapy for borderline resectable and locally advanced pancreatic ductal adenocarcinoma. JAMA Surg. 2019;154:932–42.
Macedo FI, Ryon E, Maithel SK, et al. Survival outcomes associated with clinical and pathological response following neoadjuvant FOLFIRINOX or gemcitabine/nab-paclitaxel chemotherapy in resected pancreatic cancer. Ann Surg. 2019;270:400–13.
Truty MJ, Kendrick ML, Nagorney DM, et al. Factors predicting response, perioperative outcomes, and survival following total neoadjuvant therapy for borderline/locally advanced pancreatic cancer. Ann Surg. 2019. https://doi.org/10.1097/SLA.0000000000003284.
Hashimoto D, Arima K, Nakagawa S, et al. Pancreatic cancer arising from the remnant pancreas after pancreatectomy: a multicenter retrospective study by the Kyushu Study Group of Clinical Cancer. J Gastroenterol. 2019;54:437–48.
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) Pancreatic Adenocarcinoma NCCN Evidence BlocksTM Version 3. 2019.
Zhou G, Liu X, Wang X, et al. Combination of preoperative CEA and CA19-9 improves prediction outcomes in patients with resectable pancreatic adenocarcinoma: results from a large follow-up cohort. Onco Targets Ther. 2017;10:1199–206.
Kim YC, Kim HJ, Park JH, et al. Can preoperative CA19-9 and CEA levels predict the resectability of patients with pancreatic adenocarcinoma? J Gastroenterol Hepatol. 2009;24:1869–75.
Hosokawa Y, Nagakawa Y, Sahara Y, et al. Serum SPan-1 is a significant risk factor for early recurrence of pancreatic cancer after curative resection. Dig Surg. 2017;34:125–32.
Kawa S, Oguchi H, Kobayashi T, et al. Elevated serum levels of Dupan-2 in pancreatic cancer patients negative for Lewis blood group phenotype. Br J Cancer. 1991;64:899–902.
Aoki S, Motoi F, Murakami Y, et al. Decreased serum carbohydrate antigen 19-9 levels after neoadjuvant therapy predict a better prognosis for patients with pancreatic adenocarcinoma: a multicenter case-control study of 240 patients. BMC Cancer. 2019;19:252.
Rieser CJ, Zenati M, Hamad A, et al. CA19-9 on postoperative surveillance in pancreatic ductal adenocarcinoma: predicting recurrence and changing prognosis over time. Ann Surg Oncol. 2018;25:3483–91.
Luo G, Liu C, Guo M, et al. Potential biomarkers in Lewis-negative patients with pancreatic cancer. Ann Surg. 2017;265:800–5.
Nakagawa S, Yamashita YI, Umezaki N, et al. Serum marker score based on Prognostic Nutrition Index, carcinoembryonic antigen, and carbohydrate antigen 19-9 is associated with recurrence for patients undergoing surgery for pancreatic ductal adenocarcinoma. Pancreas. 2018;47:1130–4.
Edge S, Byrd DR, Compton CC, et al. AJCC cancer staging manual. 7th ed. Springer, New York, NY, 2010.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Kang CM, Kim JY, Choi GH, et al. The use of adjusted preoperative CA 19-9 to predict the recurrence of resectable pancreatic cancer. J Surg Res. 2007;140:31–5.
Neoptolemos JP, Palmer DH, Ghaneh P, et al. Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): a multicentre, open-label, randomised, phase 3 trial. Lancet. 2017;389:1011–24.
Oettle H, Neuhaus P, Hochhaus A, et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA. 2013;310:1473–81.
Brahmer JR, Tykodi SS, Chow LQ, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366:2455–65.
Knudsen ES, Vail P, Balaji U, et al. Stratification of pancreatic ductal adenocarcinoma: combinatorial genetic, stromal, and immunologic markers. Clin Cancer Res. 2017;23:4429–40.
Mahajan UM, Langhoff E, Goni E, et al. Immune cell and stromal signature associated with progression-free survival of patients with resected pancreatic ductal adenocarcinoma. Gastroenterology. 2018;155:1625–39.e1622.
Tsukamoto M, Imai K, Ishimoto T, et al. PD-L1 expression enhancement by infiltrating macrophage-derived tumor necrosis factor-alpha leads to poor pancreatic cancer prognosis. Cancer Sci. 2019;110:310–20.
Mace TA, Shakya R, Pitarresi JR, et al. IL-6 and PD-L1 antibody blockade combination therapy reduces tumour progression in murine models of pancreatic cancer. Gut. 2018;67:320–32.
Lu C, Paschall AV, Shi H, et al. The MLL1-H3K4me3 axis-mediated PD-L1 expression and pancreatic cancer immune evasion. J Natl Cancer Inst. 2017;109:djw283.
Cassinotto C, Chong J, Zogopoulos G, et al. Resectable pancreatic adenocarcinoma: role of CT quantitative imaging biomarkers for predicting pathology and patient outcomes. Eur J Radiol. 2017;90:152–8.
Cheng SH, Cheng YJ, Jin ZY, Xue HD. Unresectable pancreatic ductal adenocarcinoma: role of CT quantitative imaging biomarkers for predicting outcomes of patients treated with chemotherapy. Eur J Radiol. 2019;113:188–97.
Xu HX, Chen T, Wang WQ, et al. Metabolic tumour burden assessed by 18F-FDG PET/CT associated with serum CA19-9 predicts pancreatic cancer outcome after resection. Eur J Nucl Med Mol Imaging. 2014;41:1093–102.
Kauhanen SP, Komar G, Seppanen MP, et al. A prospective diagnostic accuracy study of 18F-fluorodeoxyglucose positron emission tomography/computed tomography, multidetector row computed tomography, and magnetic resonance imaging in primary diagnosis and staging of pancreatic cancer. Ann Surg. 2009;250:957–63.
Kurahara H, Maemura K, Mataki Y, et al. Significance of 18F-fluorodeoxyglucose (FDG) uptake in response to chemoradiotherapy for pancreatic cancer. Ann Surg Oncol. 2019;26:644–51.
Ramanathan RK, Goldstein D, Korn RL, et al. Positron emission tomography response evaluation from a randomized phase III trial of weekly nab-paclitaxel plus gemcitabine versus gemcitabine alone for patients with metastatic adenocarcinoma of the pancreas. Ann Oncol. 2016;27:648–53.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Figure 1
Figure shows the relapse-free survival (RFS) and overall survival (OS) curve in PDAC patients with pancreatic resection according to the Pre TI. The patients with a Pre TI score 2 and 3 demonstrated significantly poorer prognoses than that of patients with a Pre TI score 0 and 1 both for RFS and OS. We excluded patients with R2 (n=5) in RFS analysis (TIFF 19784 kb)
Supplementary Figure 2
Figure shows the ROC curves for recurrence in PDAC patients according to several tumor markers. The AUC value of the Pre TI was 0.6792, which was better than that of other tumor markers, including adjusted CA19-9 (AUC=0.6118). We excluded patients with R2 (n=5) in this analysis (TIFF 19784 kb)
Supplementary Figure 3
Figure shows the relapse-free survival (RFS) and overall survival (OS) curve in PDAC patients with normal adjusted CA19-9 values after curative pancreatic resection according to the Pre TI. The patients with a Pre TI score 2 and 3 demonstrated significantly worse prognosis than that of patients with a Pre TI score 0 both for RFS (Log-rank P=0.003) and OS (Log-rank P=0.043). We excluded patients with R2 (n=2) in RFS analysis (TIFF 19784 kb)
Rights and permissions
About this article
Cite this article
Miyata, T., Hayashi, H., Yamashita, Yi. et al. Prognostic Value of the Preoperative Tumor Marker Index in Resected Pancreatic Ductal Adenocarcinoma: A Retrospective Single-Institution Study. Ann Surg Oncol 28, 1572–1580 (2021). https://doi.org/10.1245/s10434-020-09022-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09022-3