Abstract
Background
Chemotherapy is increasingly used before hepatic resection, with controversial impact regarding liver function. This study aimed to assess the capacity of 99mTc-labelled-mebrofenin SPECT-hepatobiliary scintigraphy (HBS) to predict liver dysfunction due to chemotherapy and/or chemotherapeutic-associated liver injuries (CALI), such as sinusoidal obstruction syndrome (SOS) and nonalcoholic steatohepatitis (NASH) activity score (NAS).
Methods
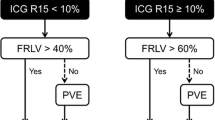
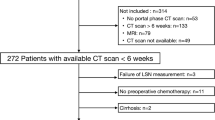
From 2011 to 2015, all consecutive noncirrhotic patients scheduled for a major hepatectomy (≥ 3 segments) gave informed consent for preoperative SPECT-HBS allowing measurements of segmental liver function. As primary endpoint, HBS results were compared between patients with versus without (1) preoperative chemotherapy (≤ 3 months); and (2) CALI, mainly steatosis, NAS (Kleiner), or SOS (Rubbia-Brandt). Secondary endpoints were (1) other factors impairing function; and (2) impact of chemotherapy, and/or CALI on hepatocyte isolation outcome via liver tissues.
Results
Among 115 patients, 55 (47.8%) received chemotherapy. Sixteen developed SOS and 35 NAS, with worse postoperative outcome. Overall, chemotherapy had no impact on liver function, except above 12 cycles. In patients with CALI, a steatosis ≥ 30% significantly compromised function, as well as NAS, especially grades 2–5. Conversely, SOS had no impact, although subjected to very low patients number with severe SOS. Other factors impairing function were diabetes, overweight/obesity, or fibrosis. Similarly, chemotherapy in 73 of 164 patients had no effect on hepatocytes isolation outcome; regarding CALI, steatosis ≥ 30% and NAS impaired the yield and/or viability of hepatocytes, but not SOS.
Conclusions
In this first large, prospective study, HBS appeared to be a valuable tool to select heavily treated patients at risk of liver dysfunction through steatosis or NAS.


Similar content being viewed by others
References
Sturesson C, Nilsson J, Eriksson S, Spelt L, Andersson R. Limiting factors for liver regeneration after a major hepatic resection for colorectal cancer metastases. HPB. 2013;15:646–52.
Sturesson C, Keussen I, Tranberg KG. Prolonged chemotherapy impairs liver regeneration after portal vein occlusion: an audit of 26 patients. Eur J Surg Oncol. 2010;36:358–64.
Goere D, Farges O, Leporrier J, Sauvanet A, Vilgrain V, Belghiti J. Chemotherapy does not impair hypertrophy of the left liver after right portal vein obstruction. J Gastrointest Surg. 2006;10:365–70.
Rickenbacher A, DeOliveira ML, Tian Y, Jang JH, Riener M, Graf R, et al. Arguments against toxic effects of chemotherapy on liver injury and regeneration in an experimental model of partial hepatectomy. Liver Int. 2011;31:313–21.
De Graaf W, Bennink RJ, Vetelainen R, van Gulik TM. Nuclear imaging techniques for the assessment of hepatic function in liver surgery and transplantation. J Nucl Med. 2010;51:742–52.
Truant S, Oberlin O, Sergent G, Lebuffe G, Gambiez L, Ernst O, et al. Remnant liver volume to body weight ratio ≥ 0.5%: a new cut-off to estimate postoperative risks after extended resection in noncirrhotic liver. J Am Coll Surg. 2007;204:22–33.
Kishi Y, Abdalla EK, Chun YS, Zorzi D, Madoff DC, Wallace MJ, et al. Three hundred and one consecutive extended right hepatectomies: evaluation of outcome based on systematic liver volumetry. Ann Surg. 2009;250:540–8.
Krishnamurthy S, Krishnamurthy GT. Technetium-99 m-iminodiacetic acid organic anions: review of biokinetics and clinical application in hepatology. Hepatology. 1989;9:139–53.
Choti M a, Sitzmann J V, Tiburi MF, Sumetchotimetha W, Rangsin R, Schulick RD, et al. Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg. 2002;235:759–66.
Welsh FK, Tilney HS, Tekkis PP, John TG, Rees M. Safe liver resection following chemotherapy for colorectal metastases is a matter of timing. Br J Cancer. 2007;96:1037–42.
Takamoto T, Hashimoto T, Sano K, Maruyama Y, Inoue K, Ogata S, et al. Recovery of liver function after the cessation of preoperative chemotherapy for colorectal liver metastasis. Ann Surg Oncol. 2010;17:2747–55.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, et al. The “50–50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg. 2005;242:824–8.
Mullen JT, Ribero D, Reddy SK, Donadon M, Zorzi D, Gautam S, et al. Hepatic insufficiency and mortality in 1,059 noncirrhotic patients undergoing major hepatectomy. J Am Coll Surg. 2007;204:854–62.
Skrzypczyk C, Truant S, Duhamel A, Langlois C, Boleslawski E, Koriche D, et al. Relevance of the ISGLS definition of posthepatectomy liver failure in early prediction of poor outcome after liver resection: study on 680 hepatectomies. Ann Surg. 2014;13:865–70.
Ekman M, Fjalling M, Holmberg S, Person H. IODIDA clearance rate: a method for measuring hepatocyte uptake function. Transpl Proc. 1992;24:387–8.
Boleslawski E, Decanter G, Truant S, Bouras AF, Sulaberidze L, Oberlin O, et al. Right hepatectomy with extra-hepatic vascular division prior to transection: intention-to-treat analysis of a standardized policy. HPB. 2012;14:688–99.
Rubbia-Brandt L, Audard V, Sartoretti P, Roth AD, Brezault C, Le Charpentier M, et al. Severe hepatic sinusoidal obstruction associated with oxaliplatin-based chemotherapy in patients with metastatic colorectal cancer. Ann Oncol. 2004;15:460–6.
Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–21.
Truant S, Bouras AF, Petrovai G, Buob D, Ernst O, Boleslawski E, et al. Volumetric gain of the liver after major hepatectomy in obese patients: a case-matched study in 84 patients. Ann Surg. 2013;258:696–704.
Vondran FW, Katenz E, Schwartlander R, Morgul MH, Raschzok N, Gong X, et al. Isolation of primary human hepatocytes after partial hepatectomy: criteria for identification of the most promising liver specimen. Artif Organs. 2008;32:205–13.
Seglen PO. Preparation of isolated rat liver cells. Methods Cell Biol. 1976;13:29–83.
Sharanek A, Burban A, Burbank M, Le Guevel R, Li R, Guillouzo A, et al. Rho-kinase/myosin light chain kinase pathway plays a key role in the impairment of bile canaliculi dynamics induced by cholestatic drugs. Sci Rep. 2016;6:24709.
Vauthey JN, Pawlik TM, Ribero D, Wu TT, Zorzi D, Hoff PM, et al. Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J Clin Oncol. 2006;24:2065–72. https://doi.org/10.1200/JCO.2005.05.3074.
Pawlik TM, Olino K, Gleisner AL, Torbenson M, Schulick R, Choti MA. Preoperative chemotherapy for colorectal liver metastases: impact on hepatic histology and postoperative outcome. J Gastrointest Surg. 2007;11:860–8.
Scoggins CR, Campbell ML, Landry CS, Slomiany BA, Woodall CE, McMasters KM, et al. Preoperative chemotherapy does not increase morbidity or mortality of hepatic resection for colorectal cancer metastases. Ann Surg Oncol. 2009;16:35–41.
Karoui M, Penna C, Amin-Hashem M, Mitry E, Benoist S, Franc B, et al. Influence of preoperative chemotherapy on the risk of major hepatectomy for colorectal liver metastases. Ann Surg. 2006;243:1–7.
Kishi Y, Zorzi D, Contreras CM, Maru DM, Kopetz S, Ribero D, et al. Extended preoperative chemotherapy does not improve pathologic response and increases postoperative liver insufficiency after hepatic resection for colorectal liver metastases. Ann Surg Oncol. 2010;17:2870–6.
Brouquet A, Benoist S, Julie C, Penna C, Beauchet A, Rougier P, et al. Risk factors for chemotherapy-associated liver injuries: A multivariate analysis of a group of 146 patients with colorectal metastases. Surgery. 2009;145:362–71.
Vigano L, De Rosa G, Toso C, Andres A, Ferrero A, Roth A, et al. Reversibility of chemotherapy-related liver injury. J Hepatol. 2017;67:84–91.
Millet G, Truant S, Leteurtre E, Hebbar M, Zerbib P, Huet G, et al. Volumetric analysis of remnant liver regeneration after major hepatectomy in bevacizumab-treated patients: a case-matched study in 82 patients. Ann Surg. 2012;256:752–5.
Pessaux P, Panaro F, Casnedi S, Zeca I, Marzano E, Bachellier P, et al. Targeted molecular therapies (cetuximab and bevacizumab) do not induce additional hepatotoxicity: Preliminary results of a case–control study. Eur J Surg Oncol. 2010;36:575–82.
Russolillo N, Langella S, Perotti S, Lo Tesoriere R, Forchino F, Ferrero A. Preoperative assessment of chemotherapeutic associated liver injury based on indocyanine green retention test. Int J Surg. 2016;31:80–5.
Wakiya T, Kudo D, Toyoki Y, Ishido K, Kimura N, Narumi S, et al. Evaluation of the usefulness of the indocyanine green clearance test for chemotherapy-associated liver injury in patients with colorectal cancer liver metastasis. Ann Surg Oncol. 2014;21:167–72. https://doi.org/10.1245/s10434-013-3203-3.
Narita M, Oussoultzoglou E, Chenard M-P, Fuchshuber P, Rather M, Rosso E, et al. Liver injury due to chemotherapy-induced sinusoidal obstruction syndrome is associated with sinusoidal capillarization. Ann Surg Oncol. 2012;19:2230–7. https://doi.org/10.1245/s10434-011-2112-6.
Nakano H, Oussoultzoglou E, Rosso E, Casnedi S, Chenard-Neu M-PP, Dufour P, et al. Sinusoidal injury increases morbidity after major hepatectomy in patients with colorectal liver metastases receiving preoperative chemotherapy. Ann Surg. 2008;247:118–24.
Aloia T, Sebagh M, Plasse M, Karam V, Levi F, Giacchetti S, et al. Liver histology and surgical outcomes after preoperative chemotherapy with fluorouracil plus oxaliplatin in colorectal cancer liver metastases. J Clin Oncol. 2006;24:4983–90.
Soubrane O, Brouquet A, Zalinski S, Terris B, Brezault C, Mallet V, et al. Predicting high grade lesions of sinusoidal obstruction syndrome related to oxaliplatin-based chemotherapy for colorectal liver metastases: correlation with post-hepatectomy outcome. Ann Surg. 2010;251:454–60.
Simpson AL, Leal JN, Pugalenthi A, Allen PJ, Dematteo RP, Fong Y, et al. Chemotherapy-induced splenic volume increase is independently associated with major complications after hepatic resection for metastatic colorectal cancer. J Am Coll Surg. 2015;220:271–80.
Schiffer E, Frossard JL, Rubbia-Brandt L, Mentha G, Pastor CM. Hepatic regeneration is decreased in a rat model of sinusoidal obstruction syndrome. J Surg Oncol. 2009;99:439–46.
Slade JH, Alattar ML, Fogelman DR, Overman MJ, Agarwal A, Maru DM, et al. Portal hypertension associated with oxaliplatin administration: clinical manifestations of hepatic sinusoidal injury. Clin Colorectal Cancer. 2009;8:225–30.
Parikh AA, Gentner B, Wu TT, Curley SA, Ellis LM, Vauthey JN. Perioperative complications in patients undergoing major liver resection with or without neoadjuvant chemotherapy. J Gastrointest Surg. 2003;7:1082–8.
Zeiss J, Merrick HW, Savolaine ER, Woldenberg LS, Kim K, Schlembach PJ. Fatty liver change as a result of hepatic artery infusion chemotherapy. Am J Clin Oncol. 1990;13:156–60.
Peppercorn PD, Reznek RH, Wilson P, Slevin ML, Gupta RK. Demonstration of hepatic steatosis by computerized tomography in patients receiving 5-fluorouracil-based therapy for advanced colorectal cancer. Br J Cancer. 1998;77:2008–11.
Rubbia-Brandt L, Lauwers GY, Wang H, Majno PE, Tanabe K, Zhu AX, et al. Sinusoidal obstruction syndrome and nodular regenerative hyperplasia are frequent oxaliplatin-associated liver lesions and partially prevented by bevacizumab in patients with hepatic colorectal metastasis. Histopathology. 2010;56:430–9.
Behrns KE, Tsiotos GG, DeSouza NF, Krishna MK, Ludwig J, Nagorney DM. Hepatic steatosis as a potential risk factor for major hepatic resection. J Gastrointest Surg. 1998;2:292–8.
Kooby DA, Fong Y, Suriawinata A, Gonen M, Allen PJ, Klimstra DS, et al. Impact of steatosis on perioperative outcome following hepatic resection. J Gastrointest Surg. 2003;7:1034–44.
Baumgaertner I, Ratziu V, Vaillant J-C, Hannoun L, Poynard T, André T. [Hepatotoxicity of metastatic colorectal cancer chemotherapy: systematic review]. Bull Cancer. 2010;97:559–69.
Salgado Júnior W, Donadelli CA de M, Dos Santos JS, Nonino CB. Influence of Roux-en-Y gastric bypass on the hepatocellular function and bile flow of obese patients assessed by scintigraphy with DISIDA. Obes Surg. 2016;26:2718–23.
Şen H, Tan YZ, Binnetoğlu E, Aşik M, Güneş F, Erbağ G, et al. Evaluation of liver perfusion in diabetic patients using 99mTc-sestamibi. Wien Klin Wochenschr. 2015;127:19–23.
Rijzewijk LJ, van der Meer RW, Lubberink M, Lamb HJ, Romijn JA, de Roos A, et al. Liver fat content in type 2 diabetes: relationship with hepatic perfusion and substrate metabolism. Diabetes. 2010;59:2747–54.
Kawahara T, Toso C, Douglas DN, Nourbakhsh M, Lewis JT, Tyrrell DL, et al. Factors affecting hepatocyte isolation, engraftment, and replication in an in vivo model. Liver Transpl. 2010;16:974–82.
Le Roux F, Herpe Y-E, Bruyer A-S, Duverlie G, Regimbeau J-M. Les résultats de la culture d’hépatocytes primaires humains peuvent-ils être prédictifs des suites opératoires après hépatectomie (Abstract). J Chir (Communication Orale). 2014:A5–35.
Hewes JC, Riddy D, Morris RW, Woodrooffe AJ, Davidson BR, Fuller B. A prospective study of isolated human hepatocyte function following liver resection for colorectal liver metastases: the effects of prior exposure to chemotherapy. J Hepatol. 2006;45:263–70.
Zhao J, van Mierlo KMC, Gómez-Ramírez J, Kim H, Pilgrim CHC, Pessaux P, et al. Systematic review of the influence of chemotherapy-associated liver injury on outcome after partial hepatectomy for colorectal liver metastases. Br J Surg. 2017;104:990–1002.
Cortez-Pinto H, Chatham J, Chacko VP, Arnold C, Rashid A, Diehl AM. Alterations in liver ATP homeostasis in human nonalcoholic steatohepatitis: a pilot study. J Am Med Assoc. 1999;282:1659–64.
Yang SQ, Mandal AK, Huang J, Diehl AM. Disrupted signaling and inhibited regeneration in obese mice with fatty livers: Implications for nonalcoholic fatty liver disease pathophysiology. Hepatology. 2001;34:694–706.
Teramoto K, Bowers JL, Kruskal JB, Clouse ME. Hepatic microcirculatory changes after reperfusion in fatty and normal liver transplantation in the rat. Transplantation. 1993;56:1076–82.
Bedossa P, Dargère D, Paradis V. Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology. 2003;38:1449–57.
Allard MA, Sebagh M, Baillie G, Lemoine A, Dartigues P, Faitot F, et al. Comparison of complete pathologic response and hepatic injuries between hepatic arterial infusion and systemic administration of oxaliplatin in patients with colorectal liver metastases. Ann Surg Oncol. 2015;22:1925–32. https://doi.org/10.1245/s10434-014-4272-7.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Truant, S., Baillet, C., Gnemmi, V. et al. The Impact of Modern Chemotherapy and Chemotherapy-Associated Liver Injuries (CALI) on Liver Function: Value of 99mTc-Labelled-Mebrofenin SPECT-Hepatobiliary Scintigraphy. Ann Surg Oncol 28, 1959–1969 (2021). https://doi.org/10.1245/s10434-020-08988-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08988-4