Abstract
Background
Modified radical mastectomy (MRM), which includes axillary dissection, is the standard of care for inflammatory breast cancer (IBC). While more limited axillary staging after neoadjuvant chemotherapy (NAC) in clinically node-positive non-IBC has been increasingly adopted, the impact of these techniques in IBC is not clear. To inform patient selection for further study of limited axillary surgery, we aimed to describe the frequency and factors associated with pathological node-negativity (ypN0) in IBC.
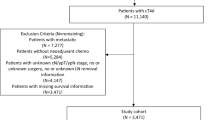
Methods
Patients with IBC who received NAC and MRM were identified from a prospective institutional database (2004–2019). Binary logistic regression analyses were conducted to identify factors associated with ypN0.
Results
Of 453 patients, 189 (41.7%) had a post-NAC clinical nodal stage (ycN stage) of N0 (ycN1: 150, 33.1%; ycN2: 4, 0.9%; ycN3: 47, 10.4%; unknown: 63, 13.9%); 156 (34%) were ypN0. On multivariable analysis, higher tumor grade was not associated with ypN0 (odds ratio [OR] 1.59, 95% confidence interval [CI] 0.90–2.81, p =0.11). Compared with hormone receptor (HR)-negative/human epidermal growth factor receptor 2 (HER2)-negative tumors (n =113, 24.9%), HR-positive/HER2-negative tumors (n =169, 37.3%) had a trend toward less ypN0 (OR 0.55, 95% CI 0.29–1.02, p =0.06); HR-positive/HER2-positive tumors (n =79, 17.4%) were similar to HR-negative/HER2-negative tumors (OR 0.72, 95% CI 0.35–1.48, p =0.37); and HR-negative/HER2-positive tumors (n =92, 20.3%) were associated with increased ypN0 (OR 4.82, 95% CI 2.41–9.63, p <0.001). As ycN stage increased, the likelihood of ypN0 decreased compared with ycN0 patients (ycN1/2: OR 0.54, 95% CI 0.32–0.89, p =0.02; ycN3: OR 0.29, 95% CI 0.13–0.67, p =0.004).
Conclusions
One-third of patients with IBC who received NAC and MRM had pathologically negative nodes. Factors associated with ypN0 included ycN0 status and HR-negative/HER2-positive subtype. Large, prospective studies are needed to investigate the feasibility of alternative nodal evaluation strategies in IBC, with consideration to these subgroups.



Similar content being viewed by others
References
Dawood S, Merajver SD, Viens P, et al. International expert panel on inflammatory breast cancer: consensus statement for standardized diagnosis and treatment. Anna. Oncol. 2011;22(3):515–23.
Anderson WF, Schairer C, Chen BE, Hance KW, Levine PH. Epidemiology of inflammatory breast cancer (IBC). Breast Dis. 2005;22:9–23.
Amin MB, Edge S, Greene F, Byrd DR, Brookland RK, Washington MK, Gershenwald JE, Compton CC, Hess KR, et al. AJCC cancer staging manual. 8th ed. Berlin: Springer; 2017.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30.
Levine PH, Zolfaghari L, Young H, et al. What is inflammatory breast cancer? Revisiting the case definition. Cancers. 2010;2(1):143–52.
Hance KW, Anderson WF, Devesa SS, Young HA, Levine PH. Trends in inflammatory breast carcinoma incidence and survival: the surveillance, epidemiology, and end results program at the National Cancer Institute. J Natl Cancer Inst. 2005;97(13):966–75.
Network NCC. Breast Cancer (Version 3.2020). https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 23 Apr 2020.
Ueno NT, Espinosa Fernandez JR, Cristofanilli M, et al. International Consensus on the Clinical Management of Inflammatory Breast Cancer from the Morgan Welch Inflammatory Breast Cancer Research Program 10th Anniversary Conference. J Cancer. 2018;9(8):1437–47.
Yamauchi H, Woodward WA, Valero V, et al. Inflammatory breast cancer: what we know and what we need to learn. Oncologist. 2012;17(7):891–9.
Lucci A, McCall LM, Beitsch PD, et al. Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American College of Surgeons Oncology Group Trial Z0011. J Clin Oncol. 2007;25(24):3657–63.
Caudle AS, Bedrosian I, Milton DR, et al. Use of sentinel lymph node dissection after neoadjuvant chemotherapy in patients with node-positive breast cancer at diagnosis: practice patterns of American Society of Breast Surgeons Members. Ann Surg Oncol. 2017;24(10):2925–34.
Mamtani A, Barrio AV, King TA, et al. How often does neoadjuvant chemotherapy avoid axillary dissection in patients with histologically confirmed nodal metastases? Results of a prospective study. Ann Surg Oncol. 2016;23(11):3467–74.
Nguyen TT, Hoskin TL, Day CN, et al. Decreasing use of axillary dissection in node-positive breast cancer patients treated with neoadjuvant chemotherapy. Ann Surg Oncol. 2018;25(9):2596–602.
Caudle AS. Intraoperative pathologic evaluation with targeted axillary dissection: Editorial for “intraoperative touch imprint cytology in targeted axillary dissection after neoadjuvant chemotherapy among breast cancer patients with initial axillary metastasis”. Ann Surg Oncol. 2018;25(11):3112–4.
Boughey JC, Suman VJ, Mittendorf EA, et al. Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer: the ACOSOG Z1071 (Alliance) clinical trial. JAMA. 2013;310(14):1455-61.
DeSnyder SM, Mittendorf EA, Le-Petross C, et al. Prospective feasibility trial of sentinel lymph node biopsy in the setting of inflammatory breast cancer. Clin Breast Cancer. 2018;18(1):e73–7.
Stearns V, Ewing CA, Slack R, Penannen MF, Hayes DF, Tsangaris TN. Sentinel lymphadenectomy after neoadjuvant chemotherapy for breast cancer may reliably represent the axilla except for inflammatory breast cancer. Ann Surg Oncol. 2002;9(3):235–42.
Hidar S, Bibi M, Gharbi O, et al. Sentinel lymph node biopsy after neoadjuvant chemotherapy in inflammatory breast cancer. Int J Surge. 2009;7(3):272–5.
Rueth NM, Lin HY, Bedrosian I, et al. Underuse of trimodality treatment affects survival for patients with inflammatory breast cancer: an analysis of treatment and survival trends from the National Cancer Database. J Clin Oncol. 2014;32(19):2018–24.
Tsai CJ, Li J, Gonzalez-Angulo AM, et al. Outcomes after multidisciplinary treatment of inflammatory breast cancer in the era of neoadjuvant HER2-directed therapy. Am J Clin Oncol. 2015;38(3):242–7.
Dawood S, Gong Y, Broglio K, et al. Trastuzumab in primary inflammatory breast cancer (IBC): high pathological response rates and improved outcome. Breast J. 2010;16(5):529–32.
Wecsler JS, Tereffe W, Pedersen RC, et al. Lymph node status in inflammatory breast cancer. Breast Cancer Res Treat. 2015;151(1):113–20.
Hennessy BT, Gonzalez-Angulo AM, Hortobagyi GN, et al. Disease-free and overall survival after pathologic complete disease remission of cytologically proven inflammatory breast carcinoma axillary lymph node metastases after primary systemic chemotherapy. Cancer. 2006;106(5):1000–6.
Fayanju OM, Ren Y, Greenup RA, et al. Extent of axillary surgery in inflammatory breast cancer: a survival analysis of 3500 patients. Breast Cancer Res Treat. 2020;180(1):207–17.
Hieken TJ, Murphy BL, Boughey JC, Degnim AC, Glazebrook KN, Hoskin TL. Influence of biologic subtype of inflammatory breast cancer on response to neoadjuvant therapy and cancer outcomes. Clin Breast Cancer. 2018;18(4):e501–6.
Gianni L, Pienkowski T, Im YH, et al. 5-year analysis of neoadjuvant pertuzumab and trastuzumab in patients with locally advanced, inflammatory, or early-stage HER2-positive breast cancer (NeoSphere): a multicentre, open-label, phase 2 randomised trial. Lancet Oncol. 2016;17(6):791–800.
Vila J, Mittendorf EA, Farante G, et al. Nomograms for predicting axillary response to neoadjuvant chemotherapy in clinically node-positive patients with breast cancer. Ann Surg Oncol. 2016;23(11):3501–9.
Cortazar P, Zhang L, Untch M, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384(9938):164–72.
Nakhlis F, Regan MM, Warren LE, et al. The impact of residual disease after preoperative systemic therapy on clinical outcomes in patients with inflammatory breast cancer. Ann Surg Oncol. 2017;24(9):2563–9.
Imeokparia FO, Hughes TM, Dossett LA, Jeruss JS, Chang AE, Sabel MS. Axillary pathologic complete response in inflammatory breast cancer patients: implications for SLNB? Ann Surg Oncol. 2019;26(10):3374–9.
Kupstas AR, Hoskin TL, Day CN, Boughey JC, Habermann EB, Hieken TJ. Biological subtype, treatment response and outcomes in inflammatory breast cancer using data from the National Cancer Database. Br J Surg. 2020;107(8):1033–41.
Masuda H, Brewer TM, Liu DD, et al. Long-term treatment efficacy in primary inflammatory breast cancer by hormonal receptor- and HER2-defined subtypes. Ann Oncol. 2014;25(2):384–91.
Shin K, Weaver O, Wei W, Caudle AS, Kuerer HM, Yang WT. Sonographic features of benign and malignant axillary nodes post-neoadjuvant chemotherapy. Breast J. 2020;26(2):182–7.
Le-Petross HT, McCall LM, Hunt KK, et al. Axillary ultrasound identifies residual nodal disease after chemotherapy: results from the American College of Surgeons Oncology Group Z1071 Trial (Alliance). AJR. Am J Roentgenol. 2018;210(3):669–76.
Yang WT, Le-Petross HT, Macapinlac H, et al. Inflammatory breast cancer: PET/CT, MRI, mammography, and sonography findings. Breast Cancer Res Treat. 2008;109(3):417–26.
Caudle AS, Kuerer HM, Krishnamurthy S, et al. Feasibility of fine-needle aspiration for assessing responses to chemotherapy in metastatic nodes marked with clips in breast cancer: a prospective registry study. Cancer. 2019;125(3):365–73.
Caretta-Weyer H, Sisney GA, Beckman C, et al. Impact of axillary ultrasound and core needle biopsy on the utility of intraoperative frozen section analysis and treatment decision making in women with invasive breast cancer. Am J Surg. 2012;204(3):308–14.
Brzezinska M, Williams LJ, Thomas J, Michael Dixon J. Outcomes of patients with inflammatory breast cancer treated by breast-conserving surgery. Breast Cancer Res Treat. 2016;160(3):387–91.
Rosso KJ, Ueno NT, Woodward WA, Lucci A. In response to “outcomes of patients with inflammatory breast cancer treated by breast conserving surgery”: the argument against breast conservation and sentinel lymph node biopsy in IBC. Breast Cancer Res Treat. 2017;165(3):779–81.
Fayanju OM, Ren Y, Thomas SM, et al. The clinical significance of breast-only and node-only pathologic complete response (pCR) after neoadjuvant chemotherapy (NACT): a review of 20,000 breast cancer patients in the National Cancer Data Base (NCDB). Ann Surg. 2018;268(4):591–601.
Rosso KJ, Tadros AB, Weiss A, et al. Improved locoregional control in a contemporary cohort of nonmetastatic inflammatory breast cancer patients undergoing surgery. Ann Surg Oncol. 2017;24(10):2981–8.
Acknowledgment
The authors appreciate the support from the Morgan Welch Inflammatory Breast Cancer Research Program and the State of Texas Rare and Aggressive Breast Cancer Research Program Grant.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Postlewait, L.M., Teshome, M., DeSnyder, S.M. et al. Factors Associated with Pathological Node Negativity in Inflammatory Breast Cancer: Are There Patients Who May be Candidates for a De-Escalation of Axillary Surgery?. Ann Surg Oncol 27, 4603–4612 (2020). https://doi.org/10.1245/s10434-020-08891-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08891-y