Abstract
Background
Neoadjuvant endocrine therapy (NET) is effective in downstaging large hormone receptor-positive (HR+) breast cancers and increasing rates of breast-conserving surgery (BCS), but data regarding nodal pathologic complete response (pCR) are sparse. We reported nodal and breast downstaging rates with NET, and compared axillary response rates following NET and neoadjuvant chemotherapy (NAC).
Methods
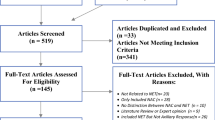
Consecutive stage I–III breast cancer patients treated with NET and surgery from January 2009 to December 2019 were identified from a prospectively maintained database. Nodal pCR rates were compared between biopsy-proven node-positive patients treated with NET, and HR+/HER2- patients treated with NAC from November 2013 to July 2019.
Results
127 cancers treated with NET and 338 with NAC were included. NET recipients were older, more likely to have lobular and lower-grade tumors, and higher HR expression. With NET, the nodal pCR rate was 11% (4/38) of biopsy-proven cases, and the breast pCR rate was 1.6% (2/126). Nodal-dowstaging rates with NET and NAC were not significantly different (11% vs 18%; P = 0.37). Patients achieving nodal pCR with NET versus NAC were older (median age 70 vs 50, P = 0.004) and had greater progesterone receptor (PR) expression (85% vs 13%, P = 0.031), respectively. Of patients not candidates for BCS due to a large tumor relative to breast size, 36/47 (77%) became BCS-eligible with NET (median PR expression 55% vs 5% in those remaining ineligible, P < 0.05).
Conclusion
Although nodal pCR is more frequent than breast pCR, NET is more likely to de-escalate breast surgery than axillary surgery. However, with a nodal pCR rate of 11%, NET remains an option for downstaging node-positive patients without clear indications for NAC.


Similar content being viewed by others
References
King TA, Morrow M. Surgical issues in patients with breast cancer receiving neoadjuvant chemotherapy. Nat Rev Clin Oncol. 2015;12:335–43.
Pariser AC, Sedghi T, Soulos PR, Killelea B, Gross CP, Mougalian SS. Utilization, duration, and outcomes of neoadjuvant endocrine therapy in the United States. Breast Cancer Res Treat. 2019;178:419–26.
Spring LM, Gupta A, Reynolds KL, et al. Neoadjuvant endocrine therapy for estrogen receptor-positive breast cancer: a systematic review and meta-analysis. JAMA Oncol. 2016;2:1477–86.
Weiss A, Wong S, Golshan M, et al. Patterns of axillary management in stages 2 and 3 hormone receptor-positive breast cancer by initial treatment approach. Ann Surg Oncol. 2019;26:4326–36.
Mamtani A, Barrio AV, King TA, et al. How often does neoadjuvant chemotherapy avoid axillary dissection in patients with histologically confirmed nodal metastases? Results of a prospective study. Ann Surg Oncol. 2016;23:3467–74.
Petruolo OA, Pilewskie M, Patil S, et al. Standard pathologic features can be used to identify a subset of estrogen receptor-positive, HER2-negative patients likely to benefit from neoadjuvant chemotherapy. Ann Surg Oncol. 2017;24:2556–62.
Laws A, Hughes ME, Hu J, et al. Impact of residual nodal disease burden on technical outcomes of sentinel lymph node biopsy for node-positive (cN1) breast cancer patients treated with neoadjuvant chemotherapy. Ann Surg Oncol. 2019;26:3846–55.
Boughey JC, McCall LM, Ballman KV, et al. Tumor biology correlates with rates of breast-conserving surgery and pathologic complete response after neoadjuvant chemotherapy for breast cancer: findings from the ACOSOG Z1071 (Alliance) Prospective Multicenter Clinical Trial. Ann Surg. 2014;260:608–14; discussion 614–606.
Pappas P TM, Rubsy J. Axillary pathology complete response rates in node positve breast cancer after neoadjuvant chemo- or endocrine therapy. Poster 522 at ABS Conference 2013. Eur J Surg Oncol. 2013;39:522.
Al Mushawah F, Tan MC, Margenthaler JA. Residual nodal disease in biopsy proven n1/n2 breast cancer following neoadjuvant systemic therapy. World J Surg. 2010;34:256–60.
Rusz O, Voros A, Varga Z, et al. One-year neoadjuvant endocrine therapy in breast cancer. Pathol Oncol Res. 2015;21:977–84.
Alba E, Chacon JI, Lluch A, et al. A randomized phase II trial of platinum salts in basal-like breast cancer patients in the neoadjuvant setting: results from the GEICAM/2006-03, multicenter study. Breast Cancer Res Treat. 2012;136:487–93.
Semiglazov VF, Semiglazov VV, Dashyan GA, et al. Phase 2 randomized trial of primary endocrine therapy versus chemotherapy in postmenopausal patients with estrogen receptor-positive breast cancer. Cancer. 2007;110:244–54.
Ellis MJ, Suman VJ, Hoog J, et al. Randomized phase II neoadjuvant comparison between letrozole, anastrozole, and exemestane for postmenopausal women with estrogen receptor-rich stage 2 to 3 breast cancer: clinical and biomarker outcomes and predictive value of the baseline PAM50-based intrinsic subtype--ACOSOG Z1031. J Clin Oncol. 2011;29:2342–9.
LeVasseur N, Willemsma KA, Li H, et al. Efficacy of neoadjuvant endocrine therapy versus neoadjuvant chemotherapy in ER-positive breast cancer: results from a prospective institutional database. Clin Breast Cancer. 2019;19:e683–9.
Saura C, Hlauschek D, Oliveira M, et al. Neoadjuvant letrozole plus taselisib versus letrozole plus placebo in postmenopausal women with oestrogen receptor-positive, HER2-negative, early-stage breast cancer (LORELEI): a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Oncol. 2019;20:1226–38.
ClinicalTrials.gov. Preoperative Fulvestrant With or Without Enzalutamide in ER+/HER2– Breast Cancer. Retrieved 25 June 2020 at https://clinicaltrials.gov/ct2/show/NCT02955394.
Cortazar P, Zhang L, Untch M, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–72.
Cristofanilli M, Gonzalez-Angulo A, Sneige N, et al. Invasive lobular carcinoma classic type: response to primary chemotherapy and survival outcomes. J Clin Oncol. 2005;23:41–8.
Thornton MJ, Williamson HV, Westbrook KE, et al. Neoadjuvant endocrine therapy versus neoadjuvant chemotherapy in node-positive invasive lobular carcinoma. Ann Surg Oncol. 2019;26:3166–77.
Fitzal F, Mittlboeck M, Steger G, et al. Neoadjuvant chemotherapy increases the rate of breast conservation in lobular-type breast cancer patients. Ann Surg Oncol. 2012;19:519–26.
Krop I, Abramson V, Colleoni M, et al. Abstract GS4–07: results from a randomized placebo-controlled phase 2 trial evaluating exemestane ± enzalutamide in patients with hormone receptor-positive breast cancer. Cancer Res. 2018;78(4 Suppl):GS4-07–GS04-07.
Carpenter R, Doughty JC, Cordiner C, et al. Optimum duration of neoadjuvant letrozole to permit breast-conserving surgery. Breast Cancer Res Treat. 2014;144:569–76.
Dixon JM, Renshaw L, Macaskill EJ, et al. Increase in response rate by prolonged treatment with neoadjuvant letrozole. Breast Cancer Res Treat. 2009;113:145–51.
Dixon JM, Renshaw L, Dixon J, Thomas J. Invasive lobular carcinoma: response to neoadjuvant letrozole therapy. Breast Cancer Res Treat. 2011;130:871–7.
Fontein DB, Charehbili A, Nortier JW, et al. Efficacy of six-month neoadjuvant endocrine therapy in postmenopausal, hormone receptor-positive breast cancer patients: a phase II trial. Eur J Cancer. 2014;50:2190–200.
Allevi G, Strina C, Andreis D, et al. Increased pathological complete response rate after a long-term neoadjuvant letrozole treatment in postmenopausal oestrogen and/or progesterone receptor-positive breast cancer. Br J Cancer. 2013;108:1587–92.
Rossi L, McCartney A, Risi E, et al. Cyclin-dependent kinase 4/6 inhibitors in neoadjuvant endocrine therapy of hormone receptor-positive breast cancer. Clin Breast Cancer. 2019;19:392–8.
Prat A, Saura C, Pascual T, et al. Ribociclib plus letrozole versus chemotherapy for postmenopausal women with hormone receptor-positive, HER2-negative, luminal B breast cancer (CORALLEEN): an open-label, multicentre, randomised, phase 2 trial. Lancet Oncol. 2020;21:33–43.
Acknowledgment
The preparation of this study was supported in part by a NIH/NCI Cancer Center Support Grant (No. P30 CA008748) to Memorial Sloan Kettering Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Monica Morrow has received speaking honoraria from Genomic Health. Dr. Giacomo Montagna was supported by the Ticino Cancer League, the Hanne Liebermann Foundation, the Fondation Ancrage, and the HEMMI-Stiftung. Dr. Komal Jhaveri has a consulting or advisory role with Novartis, Pfizer, Genentech, Lilly Pharmaceuticals, Astra Zeneca, Bristol-Myers Squibb, ADC Therapeutics, Taiho Oncology, Jounce Therapeutics, and Abbvie, and research funding (to the institution) from Pfizer, Genentech, Novartis, Lilly Pharmaceuticals, Astra Zeneca, Immunomedics, Puma Biotechnology, Novita Pharmaceuticals, ADC Therapeutics, Zymeworks, Debio Pharmaceuticals, and Clovis Oncology. The remaining authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Accepted for an oral presentation in poster format at the 21st Annual Meeting of the American Society of Breast Surgeons, 2020 held virtually on the 23rd of May 2020.
Rights and permissions
About this article
Cite this article
Montagna, G., Sevilimedu, V., Fornier, M. et al. How Effective is Neoadjuvant Endocrine Therapy (NET) in Downstaging the Axilla and Achieving Breast-Conserving Surgery?. Ann Surg Oncol 27, 4702–4710 (2020). https://doi.org/10.1245/s10434-020-08888-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08888-7