Abstract
Background
Several inflammation-based prognostic scores have a prognostic value in patients with various cancers. This study investigated the prognostic value of various inflammation-based prognostic scores in patients who underwent a surgery for adenocarcinoma of the esophagogastric junction (AEG) and upper gastric cancer (UGC).
Methods
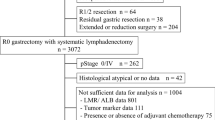
We reviewed data of 206 patients who underwent surgery for AEG and UGC. We calculated neutrophil–lymphocyte ratio (NLR), platelet–lymphocyte ratio (PLR), Glasgow Prognostic Score (GPS), modified GPS (mGPS), C-reactive protein (CRP)/albumin (Alb) ratio, prognostic index (PI), and prognostic nutritional index (PNI) and analyzed the relationship between these biomarkers and postoperative prognosis.
Results
In multivariate analyses for overall survival, mGPS (P = 0.0337, hazard ratio [HR] = 5.211), PI (P = 0.0002, HR = 21.20), and PNI (P < 0.0001, HR = 6.907) were identified as independent predictive factors. A multivariate analysis for recurrence-free survival showed that only PI (P = 0.0006, HR = 11.89) and PNI (P = 0.0002, HR = 4.972) were independent predictive factors among the above-mentioned inflammation-based prognostic scores.
Conclusions
In various inflammation-based prognostic scores, PI and PNI were more strongly associated with poor prognosis in patients who underwent surgery for AEG and UGC.



Similar content being viewed by others
References
Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108.
Lu J, Zheng CH, Cao LL, et al. The effectiveness of the 8th American joint committee on cancer TNM classification in the prognosis evaluation of gastric cancer patients: a comparative study between the 7th and 8th editions. Eur J Surg Oncol. 2017;43(12):2349–56.
Jomrich G, Hollenstein M, John M, et al. The modified Glasgow prognostic score is an independent prognostic indicator in neoadjuvantly treated adenocarcinoma of the esophagogastric junction. Oncotarget. 2018;9(6):6968–76.
Park JH, Watt DG, Roxburgh CS, et al. Colorectal cancer, systemic inflammation, and outcome: Staging the tumor and staging the host. Ann Surg. 2016;263:326–36.
Roxburgh CS, McMillan DC. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol. 2010;6:149–63.
Kudou K, Saeki H, Nakashima Y, et al. Postoperative skeletal muscle loss predicts poor prognosis of adenocarcinoma of upper stomach and esophagogastric junction. World J Surg. 2018; https://doi.org/10.1007/s00268-018-4873-6.
Tamandl D, Paireder M, Asari R, et al. Markers of sarcopenia quantified by computed tomography predict adverse long-term outcome in patients with resected oesophageal or gastro-oesophageal junction cancer. Eur Radiol. 2016;26:1359–67.
Vayrynen JP, Tuomisto A, Klintrup K, et al. Detailed analysis of inflammatory cell infiltration in colorectal cancer. Br J Cancer. 2013;109:1839–47.
Miyamoto Y, Baba Y, Sakamoto Y, et al. Sarcopenia is a negative prognostic factor after curative resection of colorectal cancer. Ann Surg Oncol. 2015;22:2663–8.
Kudou K, Saeki H, Nakashima Y, et al. Prognostic significance of sarcopenia in patients with esophagogastric junction cancer or upper gastric cancer. Ann Surg Oncol. 2017;24(7):1804–10.
Kinoshita A, Onoda H, Imai N, et al. Comparison of the prognostic value of inflammation-based prognostic scores in patients with hepatocellular carcinoma. Br J Cancer. 2012;107(6):988–93.
Ignacio de Ulibarri J, Gonzalez-Madrono A, et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. 2005;20:38–45.
Yamanaka T, Matsumoto S, Teramukai S, et al. The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Oncology. 2007;73(3–4):215–20.
Pan QX, Su ZJ, Zhang JH, et al. A comparison of the prognostic value of preoperative inflammation-based scores and TNM stage in patients with gastric cancer. Onco Targets Ther. 2015;8:1375–85.
Kuroda D, Sawayama H, Kurashige J, et al. Controlling nutritional status (CONUT) score is a prognostic marker for gastric cancer patients after curative resection. Gastric Cancer. 2017; https://doi.org/10.1007/s10120-017-0744-3.
Melling N, Gruning A, Tachezy M, et al. Glasgow Prognostic Score may be a prognostic index for overall and perioperative survival in gastric cancer without perioperative treatment. Surgery. 2016;159:1548–56.
Yu X, Wen Y, Lin Y, et al. The value of preoperative Glasgow Prognostic Score and the C-reactive protein to albumin ratio as prognostic factors for long-term survival in pathological T1N0 esophageal squamous cell carcinoma. J Cancer. 2018;9(5):807–15.
Gao GD, Sun B, Wang XB, et al. Neutrophil to lymphocyte ratio as prognostic indicator for patients with esophageal squamous cell cancer. Int J Biol Markers. 2017;32(4):e409–14.
Hirahara N, Tajima Y, Fujii Y, et al. Prognostic nutritional index as a predictor of survival in resectable gastric cancer patients with normal preoperative serum carcinoembryonic antigen levels: a propensity score matching analysis. BMC Cancer. 2018;18(1):285.
Iseki Y, Shibutani M, Maeda K, et al. Impact of the preoperative controlling nutritional status (CONUT) score on the survival after curative surgery for colorectal cancer. PLoS One. 2015;10(7):e0132488.
Lu C, Gao P, Yang Y, et al. Prognostic evaluation of platelet to lymphocyte ratio in patients with colorectal cancer. Oncotarget. 2017;8(49):86287–95.
Kudou K, Saeki H, Nakashima Y, et al. C-reactive protein/albumin ratio is a poor prognostic factor of esophagogastric junction and upper gastric cancer. J Gastroenterol Hepatol. 2018; https://doi.org/10.1111/jgh.14442.
Siewert JR, Stein HJ. Carcinoma of the cardia: Carcinoma of the gastroesophageal junction-classification, pathology and extent of resection. Dis Esophagus. 1996;9:173–82.
Han WX, Chen ZM, Wei ZJ, et al. Preoperative pre-albumin predicts prognosis of patients after gastrectomy for adenocarcinoma of esophagogastric junction. World J Surg Oncol. 2016;14(1):279.
Zhang L, Su Y, Chen Z, et al. The prognostic value of preoperative inflammation-based prognostic scores and nutritional status for overall survival in resected patients with nonmetastatic Siewert type II/III adenocarcinoma of esophagogastric junction. Medicine (Baltimore). 2017;96(30):e7647.
Toyokawa T, Muguruma K, Tamura T, et al. Comparison of the prognostic impact and combination of preoperative inflammation-based and/or nutritional markers in patients with stage II gastric cancer. Oncotarget. 2018;9(50):29351–64.
Wen J, Bedford M, Begum R, et al. The value of inflammation based prognostic scores in patients undergoing surgical resection for oesophageal and gastric carcinoma. J Surg Oncol. 2018; 117(8):1697–707.
Aggarwal BB, Gehlot P. Inflammation and cancer: how friendly is the relationship for cancer patients? Curr Opin Pharmacol. 2009;9(4):351–69.
Crumley AB, Stuart RC, McKernan M, et al. Is hypoalbuminemia an independent prognostic factor in patients with gastric cancer? World J Surg. 2010;34(10):2393–8.
Lindenmann J, Fink-Neuboeck N, Koesslbacher M, et al. The influence of elevated levels of C-reactive protein and hypoalbuminemia on survival in patients with advanced inoperable esophageal cancer undergoing palliative treatment. J Surg Oncol. 2014;110:645–50.
Espinosa E, Feliu J, Zamora P, et al. Serum albumin and other prognostic factors related to response and survival in patients with advanced non–small cell lung cancer. Lung Cancer. 1995;12(1–2):67–76.
Asher V., Lee J., Bali A. Preoperative serum albumin is an independent prognostic predictor of survival in ovarian cancer. Med Oncol. 2012;29(3):2005–9.
Borda F, Borda A, Jimenez J, et al. Predictive value of pre-treatment hypoalbuminemia in prognosis of resected colorectal cancer. Gastroenterol Hepatol. 2014;37(5):289–95.
Ray-Coquard I, Cropet C, Van Glabbeke M, et al. Lymphopenia as a prognostic factor for overall survival in advanced carcinomas, sarcomas, and lymphomas. Cancer Res. 2009;69:5383–91.
Aoi W, Naito Y, Takagi T, et al. A novel myokine, secreted protein acidic and rich in cysteine (SPARC), suppresses colon tumorigenesis via regular exercise. Gut. 2013;62(6):882–9.
Hojman P, Dethlefsen C, Brandt C, et al. Exercise-induced muscle-derived cytokines inhibit mammary cancer cell growth. Am J Phys. Endocrinol Metab. 2011;301(3):E504–10.
Acknowledgment
The authors thank Editage Group (https://www.editage.jp/) for editing the draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare that they have no conflict of interest.
Ethical Standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
Informed Consent
Informed consent to be included in the study, or the equivalent, was obtained from all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
10434_2020_8821_MOESM1_ESM.tif
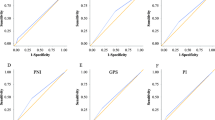
Supplementary Fig. 1. Comparison of the predictive ability of seven inflammation-based prognostic scores—NLR, PLR, GPS, mGPS, CRP/Alb ratio, PI, and PNI—by receiver operating characteristic (ROC) curve analyses. NLR neutrophil–lymphocyte ratio; PLR platelet-lymphocyte ratio; GPS Glasgow prognostic score; mGPS modified Glasgow prognostic score; CRP C-reactive protein; Alb albumin; PI prognostic index; PNI prognostic nutritional index (TIFF 29297 kb)
10434_2020_8821_MOESM2_ESM.tif
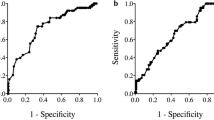
Supplementary Fig. 2 Comparison of the predictive ability of seven inflammation-based prognostic scores—NLR, PLR, GPS, mGPS, CRP/Alb ratio, PI, and PNI—by time-dependent receiver operating characteristic (ROC) curve analyses for (a) recurrence-free survival and (b) overall survival. NLR neutrophil–lymphocyte ratio; PLR platelet-lymphocyte ratio; GPS Glasgow prognostic score; mGPS modified Glasgow prognostic score; CRP C-reactive protein; Alb albumin; PI prognostic index; PNI prognostic nutritional index (TIFF 29297 kb)
10434_2020_8821_MOESM3_ESM.tif
Supplementary Fig. 3 Postoperative survival in patients with AEG and UGC based on prognostic index (PI). The Kaplan–Meier method was performed separately by tumor location. (a) Recurrence-free and (b) overall survival in patients with AEG. (c) Recurrence-free and (d) overall survival in patients with UGC. Kaplan–Meier analyses were performed according to the same criteria as in Fig. 1. AEG adenocarcinoma of esophagogastric junction; UGC upper gastric cancer; PI prognostic index(TIFF 29297 kb)
10434_2020_8821_MOESM4_ESM.tif
Supplementary Fig. 4 Postoperative survival in patients with AEG based on prognostic index (PI). The Kaplan–Meier method was performed separately by tumor location according to Siewert classification. (a) Recurrence-free and (b) overall survival in patients with Siewert type I. (c) Recurrence-free and (d) overall survival in patients with Siewert type II. (e) Recurrence-free and (f) overall survival in patients with Siewert type III. Kaplan–Meier analyses were performed according to the same criteria as in Fig. 1. AEG adenocarcinoma of esophagogastric junction; PI prognostic index (TIFF 29297 kb)
10434_2020_8821_MOESM5_ESM.tif
Supplementary Fig. 5 Postoperative survival in patients with AEG and UGC based on prognostic nutritional index (PNI). The Kaplan–Meier method was performed separately by tumor location. (a) Recurrence-free and (b) overall survival in patients with AEG. (c) Recurrence-free and (d) overall survival in patients with UGC. Kaplan–Meier analyses were performed according to the same criteria as in Fig. 2. AEG adenocarcinoma of esophagogastric junction; UGC upper gastric cancer; PNI prognostic nutritional index (TIFF 29297 kb)
10434_2020_8821_MOESM6_ESM.tif
Supplementary Fig. 6 Postoperative survival in patients with AEG based on prognostic nutritional index (PNI). The Kaplan–Meier method was performed separately by tumor location according to Siewert classification. (a) Recurrence-free and (b) overall survival in patients with Siewert type I. (c) Recurrence-free and (d) overall survival in patients with Siewert type II. (e) Recurrence-free and (f) overall survival in patients with Siewert type III. Kaplan–Meier analyses were performed according to the same criteria as in Fig. 2. AEG adenocarcinoma of esophagogastric junction; PNI prognostic nutritional index (TIFF 29297 kb)
Rights and permissions
About this article
Cite this article
Kudou, K., Nakashima, Y., Haruta, Y. et al. Comparison of Inflammation-Based Prognostic Scores Associated with the Prognostic Impact of Adenocarcinoma of Esophagogastric Junction and Upper Gastric Cancer. Ann Surg Oncol 28, 2059–2067 (2021). https://doi.org/10.1245/s10434-020-08821-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08821-y