Abstract
Background
The American College of Surgeons Oncology Group (ACOSOG) Z0011 trial demonstrated the safety of omitting axillary lymph node dissection (ALND) in T1–T2cN0 patients with fewer than three positive sentinel nodes (SLNs) undergoing breast-conservation therapy. While microscopic extracapsular extension (mECE) > 2 mm is associated with increased nodal burden, the significance of extranodal tumor deposits (ETDs) in the axillary fat is uncertain.
Methods
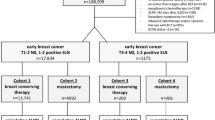
Consecutive patients with T1–T2cN0 breast cancer undergoing sentinel node biopsy and ALND for SLN metastases from January 2010 to December 2018 were identified. ETDs were defined as intravascular tumor emboli or metastatic deposits in the axillary fat. Clinicopathologic characteristics and nodal burden were compared by ETD status.
Results
Among 1114 patients, 113 (10%) had ETDs: 81 (72%) were intravascular tumor emboli and 32 (28%) were soft tissue deposits. Patients with ETDs had larger tumors (median 2.2 vs. 2.1 cm; p = 0.033) and more often had mECE (83% vs. 44%; p < 0.001). On univariable analysis, presence of ETDs (odds ratio [OR] 9.66, 95% confidence interval [CI] 6.36–14.68), larger tumors (OR 1.47, 95% CI 1.25–1.72), and mECE (OR 10.73, 95% CI 6.86–16.78) were associated with four or more additional positive non-SLNs (NSLNs; all p < 0.001). On multivariable analysis, ETDs remained associated with four or more positive NSLNs (OR 5.67, 95% CI 3.53–9.08; p < 0.001). ETDs were strongly associated with four or more positive NSLNs (OR 7.15, 95% CI 4.04–12.67) among patients with one to two positive SLNs (n = 925).
Conclusions
Among T1–T2cN0 patients with SLN metastases, ETDs are strongly associated with four or more positive NSLNs at ALND. Even among those who may otherwise meet the criteria for omission of ALND, the presence of ETDs in axillary fat warrants consideration of ALND.

Similar content being viewed by others
References
Giuliano AE, Ballman KV, McCall L, et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA. 2017;318(10):918-926.
Donker M, van Tienhoven G, Straver ME, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol. 2014;15(12):1303–1310.
Gooch J, King TA, Eaton A, et al. The extent of extracapsular extension may influence the need for axillary lymph node dissection in patients with T1–T2 breast cancer. Ann Surg Oncol. 2014;21(9):2897–2903.
Barrio AV, Downs-Canner S, Edelweiss M, et al. Microscopic extracapsular extension in sentinel lymph nodes does not mandate axillary dissection in Z0011-eligible patients. Ann Surg Oncol. 2020;27(5):1617–24.
Van Zee KJ, Manasseh DM, Bevilacqua JL, et al. A nomogram for predicting the likelihood of additional nodal metastases in breast cancer patients with a positive sentinel node biopsy. Ann Surg Oncol. 2003;10(10):1140–51.
Mittendorf EA, Hunt KK, Boughey JC, et al. Incorporation of sentinel lymph node metastasis size into a nomogram predicting nonsentinel lymph node involvement in breast cancer patients with a positive sentinel lymph node. Ann Surg. 2012;255(1):109–15.
Kwon Y, Ro J, Kang HS, et al. Clinicopathological parameters and biological markers predicting non-sentinel node metastasis in sentinel node-positive breast cancer patients. Oncol Rep. 2011;25(4):1063–71.
Katz A, Smith BL, Golshan M, et al. Nomogram for the prediction of having four or more involved nodes for sentinel lymph node-positive breast cancer. J Clin Oncol. 2008;26(13):2093–8.
Abdessalam SF, Zervos EE, Prasad M, et al. Predictors of positive axillary lymph nodes after sentinel lymph node biopsy in breast cancer. Am J Surg. 2001;182(4):316–20.
van la Parra RF, Peer PG, de Roos WK, Ernst MF, de Wilt JH, Bosscha K. A simple risk score to predict the presence of non-sentinel lymph node metastases in breast cancer patients with a positive sentinel node. World J Surg. 2014;38(5):1070–6.
Unal B, Gur AS, Beriwal S, et al. Predicting likelihood of having four or more positive nodes in patient with sentinel lymph node-positive breast cancer: a nomogram validation study. Int J Radiat Oncol Biol Phys. 2009;75(4):1035–40.
Bucci JA, Kennedy CW, Burn J, et al. Implications of extranodal spread in node positive breast cancer: a review of survival and local recurrence. Breast. 2001;10(3):213–9.
Kanyilmaz G, Findik S, Yavuz BB, Aktan M. The significance of extent of extracapsular extension in patients with T1-2 and N1 breast cancer. Eur J Breast Health. 2018;14(4):218–24.
Altinyollar H, Berberoglu U, Gulben K, Irkin F. The correlation of extranodal invasion with other prognostic parameters in lymph node positive breast cancer. J Surg Oncol. 2007;95(7):567–71.
Gorgulu S, Can MF, Yagci G, Sahin M, Tufan T. Extracapsular extension is associated with increased ratio of metastatic to examined lymph nodes in axillary node-positive breast cancer. Clin Breast Cancer. 2007;7(10):796–800.
Meretoja TJ, Audisio RA, Heikkila PS, et al. International multicenter tool to predict the risk of four or more tumor-positive axillary lymph nodes in breast cancer patients with sentinel node macrometastases. Breast Cancer Res Treat. 2013;138(3):817–27.
Vane MLG, Willemsen MA, van Roozendaal LM, et al. Extracapsular extension in the positive sentinel lymph node: a marker of poor prognosis in cT1–2N0 breast cancer patients? Breast Cancer Res Treat. 2019;174(3):711–8.
Giuliano AE, McCall L, Beitsch P, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Ann Surg. 2010;252(3):426–32 (discussion 432–423).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The preparation of this study was supported in part by NIH/NCI Cancer Center Support Grant No. P30 CA008748 to Memorial Sloan Kettering Cancer Center. Dr. Monica Morrow has received honoraria from Genomic Health; Dr. Andrea V. Barrio has received honoraria from Roche; and Debra Goldman owns stock in Johnson & Johnson unrelated to the study presented here. Anita Mamtani, Hannah Y. Wen, and Alain Vincent have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mamtani, A., Barrio, A.V., Goldman, D.A. et al. Extranodal Tumor Deposits in the Axillary Fat Indicate the Need for Axillary Dissection Among T1–T2cN0 Patients with Positive Sentinel Nodes. Ann Surg Oncol 27, 3585–3592 (2020). https://doi.org/10.1245/s10434-020-08632-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08632-1