Abstract
Background
The effect of cetuximab plus mFOLFOX on downsizing of the tumors for curative resection has yet to be assessed for patients with advanced colorectal liver metastases (CRLMs). This study aimed to assess the oncologic benefit of cetuximab plus mFOLFOX for wild-type KRAS patients with advanced CRLMs.
Methods
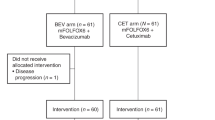
In this multicenter phase 2 trial, patients with technically unresectable tumor and/or five or more CRLMs harboring wild-type KRAS were treated with mFOLFOX plus cetuximab. The patients were assessed for resectability after 4 treatments, and then every 2 months up to 12 treatments. Patients with resectable disease were offered surgery after a waiting period of 1 month. The primary end point of the study was the R0 resection rate. The secondary end points were safety, progression-free survival (PFS), and overall survival (OS). The study is registered with the University Hospital Medical Information Network-Clinical Trials Registry Clinical Trials Registry (no. C000007923).
Results
Between 2012 and 2015, 50 patients from 13 centers were enrolled in this trial. Two patients were excluded because they had not received induction therapy. The 48 patients had a complete response rate of 0% and a partial response rate of 64.6%. For 26 R0 resections (54.2%) and 5 R1 resections (10.4%), no mortality occurred. During a median follow-up period of 31 months, the median OS for all the patients was calculated to be 41 months (95% confidence interval, 28–not reached). The 3-year OS rate was 59%.
Conclusion
For patients with advanced CRLMs harboring wild-type KRAS, cetuximab administered in combination with mFOLFOX yields high response rates, leading to significantly high R0 resection rates and favorable prognoses.



Similar content being viewed by others
References
Scheele J, Stangl R, Altendorf-Hofmann A. Hepatic metastases from colorectal carcinoma: impact of surgical resection on the natural history. Br J Surg. 1990;77:1241–6.
Kopetz S, Chang GJ, Overman MJ, et al. Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol. 2009;27:3677–83.
Adam R, Wicherts DA, de Haas RJ, et al. Patients with initially unresectable colorectal liver metastases: is there a possibility of cure? J Clin Oncol. 2009;27:1829–35.
Ashwin K. 360A. Assessment of tumour response and resection rates in unresectable metastatic colorectal liver metastases following cetuximab with neoadjuvant chemotherapy. Eur J Surg Oncol. 2014;40:S139.
Bokemeyer C, Bondarenko I, Makhson A, et al. Fluorouracil, leucovorin, and oxaliplatin with and without cetuximab in the first-line treatment of metastatic colorectal cancer. J Clin Oncol. 2009;27:663–71.
Cai S, Zhang W, Li W, et al. 598P cetuximab plus mFOLFOX-6 as first-line therapy for patients with KRAS wild-type unresectable colorectal liver-limited metastases: an open, non-randomized, multicenter phase 2 clinical trial (CLIME study). Ann Oncol. 2014;25(Suppl 4):iv204–iv204.
Folprecht G, Gruenberger T, Bechstein W, et al. Survival of patients with initially unresectable colorectal liver metastases treated with FOLFOX/cetuximab or FOLFIRI/cetuximab in a multidisciplinary concept (CELIM study). Ann Oncol. 2014;25:1018–25.
Hatano E, Okuno M, Nakamura K, et al. Conversion to complete resection with mFOLFOX6 with bevacizumab or cetuximab based on K-ras status for unresectable colorectal liver metastasis (BECK study). J Hepatobil Pancreat Sci. 2015;22:634–45.
Kohne C, Bokemeyer C, Heeger S, Sartorius U, Rougier P, Cutsem EV. Efficacy of chemotherapy plus cetuximab according to metastatic site in KRAS wild-type metastatic colorectal cancer (mCRC): analysis of CRYSTAL and OPUS studies. J Clin Oncol. 2011;29(15 Suppl):3576–3576.
Ye LC, Liu TS, Ren L, et al. Randomized controlled trial of cetuximab plus chemotherapy for patients with KRAS wild-type unresectable colorectal liver-limited metastases. J Clin Oncol. 2013;31:1931–8.
Heinemann V, von Weikersthal LF, Decker T, et al. FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer (FIRE-3): a randomised, open-label, phase 3 trial. Lancet Oncol. 2014;15:1065–75.
Schwartzberg LS, Rivera F, Karthaus M, et al. PEAK: a randomized, multicenter phase II study of panitumumab plus modified fluorouracil, leucovorin, and oxaliplatin (mFOLFOX6) or bevacizumab plus mFOLFOX6 in patients with previously untreated, unresectable, wild-type KRAS exon 2 metastatic colorectal cancer. J Clin Oncol. 2014;32:2240–7.
Lenz H, Niedzwiecki D, Innocenti F, et al. 501 OCALGB/SWOG 80405: phase III trial of irinotecan/5-FU/leucovorin (FOLFIRI) or oxaliplatin/5-FU/leucovorin (MFOLFOX6) with bevacizumab (BV) or cetuximab (CET) for patients (pts) with expanded RAS analyses untreated metastatic adenocarcinoma of the colon or rectum (MCRC). Ann Oncol. 2014;25(Suppl 4):mdu438.413-mdu438.413.
Poston G, Adam R, Xu J, et al. The role of cetuximab in converting initially unresectable colorectal cancer liver metastases for resection. Eur J Surg Oncol. 2017;43:2001–11.
Adam R, De Gramont A, Figueras J, et al. The oncosurgery approach to managing liver metastases from colorectal cancer: a multidisciplinary international consensus. Oncologist. 2012;17:1225–39.
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Folprecht G, Gruenberger T, Bechstein WO, et al. Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol. 2010;11:38–47.
Jones RP, Vauthey JN, Adam R, et al. Effect of specialist decision-making on treatment strategies for colorectal liver metastases. Br J Surg. 2012;99:1263–9.
Vallance AE, vanderMeulen J, Kuryba A, et al. Impact of hepatobiliary service centralization on treatment and outcomes in patients with colorectal cancer and liver metastases. Br J Surg. 2017;104:918–25.
Weledji EP. Centralization of liver cancer surgery and impact on multidisciplinary teams working on stage IV colorectal cancer. Oncol Rev. 2017;11:331.
Van Cutsem E, Kohne CH, Lang I, et al. Cetuximab plus irinotecan, fluorouracil, and leucovorin as first-line treatment for metastatic colorectal cancer: updated analysis of overall survival according to tumor KRAS and BRAF mutation status. J Clin Oncol. 2011;29:2011–9.
Kishi Y, Zorzi D, Contreras CM, et al. Extended preoperative chemotherapy does not improve pathologic response and increases postoperative liver insufficiency after hepatic resection for colorectal liver metastases. Ann Surg Oncol. 2010;17:2870–6.
Aloia T, Sebagh M, Plasse M, et al. Liver histology and surgical outcomes after preoperative chemotherapy with fluorouracil plus oxaliplatin in colorectal cancer liver metastases. J Clin Oncol. 2006;24:4983–90.
Memeo R, de Blasi V, Adam R, et al. Parenchymal-sparing hepatectomies (PSH) for bilobar colorectal liver metastases are associated with a lower morbidity and similar oncological results: a propensity score-matching analysis. HPB Oxford. 2016;18:781–90.
Gold JS, Are C, Kornprat P, et al. Increased use of parenchymal-sparing surgery for bilateral liver metastases from colorectal cancer is associated with improved mortality without change in oncologic outcome: trends in treatment over time in 440 patients. Ann Surg. 2008;247:109–17.
Mise Y, Aloia TA, Brudvik KW, Schwarz L, Vauthey JN, Conrad C. Parenchymal-sparing hepatectomy in colorectal liver metastasis improves salvageability and survival. Ann Surg. 2016;263:146–52.
Alberts SR, Sargent DJ, Nair S, et al. Effect of oxaliplatin, fluorouracil, and leucovorin with or without cetuximab on survival among patients with resected stage III colon cancer: a randomized trial. JAMA. 2012;307:1383–93.
Primrose J, Falk S, Finch-Jones M, et al. Systemic chemotherapy with or without cetuximab in patients with resectable colorectal liver metastasis: the New EPOC randomised controlled trial. Lancet Oncol. 2014;15:601–11.
Nordlinger B, Poston GJ, Goldberg RM. Should the results of the new EPOC trial change practice in the management of patients with resectable metastatic colorectal cancer confined to the liver? J Clin Oncol. 2015;33:241–3.
Oba M, Hasegawa K, Matsuyama Y, et al. Discrepancy between recurrence-free survival and overall survival in patients with resectable colorectal liver metastases: a potential surrogate endpoint for time to surgical failure. Ann Surg Oncol. 2014;21(6):1817–24.
Ji JH, Park SH, Lee J, et al. Prospective phase II study of neoadjuvant FOLFOX6 plus cetuximab in patients with colorectal cancer and unresectable liver-only metastasis. Cancer Chemother Pharmacol. 2013;72(1):223–30.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Eiji Shinozaki received honoraria from Merck Biopharm for lecture. All other authors declared no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mise, Y., Hasegawa, K., Saiura, A. et al. A Multicenter Phase 2 Trial to Evaluate the Efficacy of mFOLFOX6 + Cetuximab as Induction Chemotherapy to Achieve R0 Surgical Resection for Advanced Colorectal Liver Metastases (NEXTO Trial). Ann Surg Oncol 27, 4188–4195 (2020). https://doi.org/10.1245/s10434-020-08627-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08627-y