Abstract
Background
Neoadjuvant chemotherapy (NAC) has been proven to increase breast-conserving surgery (BCS) rates, but data are limited on conversion rates from BCS-ineligible (BCSi) to BCS-eligible (BCSe), specifically, in patients with large tumors.
Methods
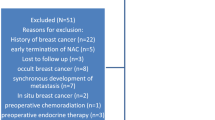
Consecutive patients with stage I–III breast cancer treated with NAC from November 2013 to March 2019 were identified. BCS eligibility before and after NAC was prospectively determined. Patients deemed BCSi before NAC due to large tumor size were studied. Statistical analyses were conducted using Student’s t-test, Wilcoxon rank sum test, Chi-square test, Fisher’s test, and logistic regression.
Results
In this study, 600 of 1353 cancers were BCSi with large tumors; 69% were non-BCS candidates, 31% were borderline-BCS (bBCS) candidates. Of non-BCS candidates, 69% became BCSe after NAC; 66% chose BCS, and 90% were successful. Among bBCS candidates, 87% were BCSe after NAC, 73% chose BCS, and 96% were successful. On univariate analysis, bBCS candidacy, lower cT stage, cN0 status, absence of calcifications, human epidermal growth factor receptor 2 positive (HER2+)/triple negative (TN) receptor status, poor differentiation, ductal histology, and breast pCR were associated with conversion to BCS eligibility. On multivariable analysis, receptor status (hormone receptor positive [HR+]/HER2– ref; odds ratio [OR] HER2+ 1.63, P = 0.047; HR–/HER2– OR, 2.26, P = 0.003) and breast pCR (OR 2.62, P < 0.001) predicted successful downstaging, while larger clinical tumor size (OR 0.86, P = 0.003), non-BCS candidacy (OR 0.46, P = 0.003), cN+ status (OR 0.54, P = 0.008), and calcifications (OR 0.56, P = 0.007) predicted lower downstaging rates.
Conclusion
In patients with large tumors precluding BCS, conversion to BCS eligibility was high with NAC, particularly in bBCS candidates. HER2+/TN receptor status predicted successful downstaging, while lower downstaging rates were observed with larger tumors, cN+ status, and calcifications. These factors should be considered when selecting patients for NAC.


Similar content being viewed by others
References
Mieog JS, van der Hage JA, van de Velde CJ. Preoperative chemotherapy for women with operable breast cancer. Cochrane Database Syst Rev. 2007(2):Cd005002.
Rastogi P, Anderson SJ, Bear HD, et al. Preoperative chemotherapy: updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J Clin Oncol. 2008;26:778–85.
Early Breast Cancer Trialists’ Group (EBCTCG). Long-term outcomes for neoadjuvant versus adjuvant chemotherapy in early breast cancer: meta-analysis of individual patient data from ten randomised trials. Lancet Oncol. 2018;19:27–39.
Boughey JC, McCall LM, Ballman KV, et al. Tumor biology correlates with rates of breast-conserving surgery and pathologic complete response after neoadjuvant chemotherapy for breast cancer: findings from the ACOSOG Z1071 (Alliance) Prospective Multicenter Clinical Trial. Ann Surg. 2014;260:608–14.
Mamtani A, Barrio AV, King TA, et al. How often does neoadjuvant chemotherapy avoid axillary dissection in patients with histologically confirmed nodal metastases? Results of a prospective study. Ann Surg Oncol. 2016;23:3467–74.
Golshan M, Cirrincione CT, Sikov WM, et al. Impact of neoadjuvant chemotherapy in stage II-III triple negative breast cancer on eligibility for breast-conserving surgery and breast conservation rates: surgical results from CALGB 40603 (Alliance). Ann Surg. 2015;262:434–9; discussion 438–9.
Golshan M, Cirrincione CT, Sikov WM, et al. Impact of neoadjuvant therapy on eligibility for and frequency of breast conservation in stage II-III HER2-positive breast cancer: surgical results of CALGB 40601 (Alliance). Breast Cancer Res Treat. 2016;160:297–304.
Boughey JC, Peintinger F, Meric-Bernstam F, et al. Impact of preoperative versus postoperative chemotherapy on the extent and number of surgical procedures in patients treated in randomized clinical trials for breast cancer. Ann Surg. 2006;244:464–70.
Fisher B, Brown A, Mamounas E, et al. Effect of preoperative chemotherapy on local-regional disease in women with operable breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-18. J Clin Oncol. 1997;15:2483–93.
van der Hage JA, van de Velde CJ, Julien JP, Tubiana-Hulin M, Vandervelden C, Duchateau L. Preoperative chemotherapy in primary operable breast cancer: results from the European Organization for Research and Treatment of Cancer trial 10902. J Clin Oncol. 2001;19:4224–37.
Golshan M, Loibl S, Wong SM, et al. Breast conservation after neoadjuvant chemotherapy for triple-negative breast cancer: surgical results from the BrighTNess Randomized Clinical Trial. JAMA Surg. 2020:e195410.
Christian N, Zabor EC, Cassidy M, Flynn J, Morrow M, Gemignani ML. Contralateral prophylactic mastectomy use after neoadjuvant chemotherapy. Ann Surg Oncol. 2020;27:743–9.
Rosenberg SM, O’Neill A, Sepucha K, et al. Abstract no. GS6-05. The Impact of Breast Cancer Surgery on Quality of Life: Long Term Results From E5103. Presented at the 41st Annual San Antonio Breast Cancer Symposium, 4–10 December 2018, San Antonio, TX, USA.
Dominici LS, Hu J, King TA, et al. Abstract no. GS6-06. Local Therapy and Quality of Life Outcomes in Young Women With Breast Cancer. Presented at the 41st Annual San Antonio Breast Cancer Symposium, 4–10 December 2018, San Antonio, TX, USA.
Adrada BE, Huo L, Lane DL, Arribas EM, Resetkova E, Yang W. Histopathologic correlation of residual mammographic microcalcifications after neoadjuvant chemotherapy for locally advanced breast cancer. Ann Surg Oncol. 2015;22:1111–7.
Feliciano Y, Mamtani A, Morrow M, Stempel MM, Patil S, Jochelson MS. Do calcifications seen on mammography after neoadjuvant chemotherapy for breast cancer always need to be excised? Ann Surg Oncol. 2017;24:1492–8.
Acknowledgments
The preparation of this manuscript was supported in part by NIH/NCI Cancer Center Support Grant No. P30 CA008748 to Memorial Sloan Kettering Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Dr. Monica Morrow has received speaking honoraria from Genomic Health. Dr. Andrea V. Barrio has received speaking honoraria from Roche. Dr. Giacomo Montagna is supported by the Ticino Cancer League, the Hanne Liebermann Foundation, the Fondation Ancrage, and the HEMMI-Stiftung. The remaining authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Accepted for presentation in podium format at the Society of Surgical Oncology 2020 International Conference on Surgical Cancer Care.
Rights and permissions
About this article
Cite this article
Petruolo, O., Sevilimedu, V., Montagna, G. et al. How Often Does Modern Neoadjuvant Chemotherapy Downstage Patients to Breast-Conserving Surgery?. Ann Surg Oncol 28, 287–294 (2021). https://doi.org/10.1245/s10434-020-08593-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08593-5