Abstract
Purpose
The current study was designed to investigate the association between the average preoperative physical activity and postoperative outcomes in patients undergoing surgeries for hepato-pancreato-biliary (HPB) malignancy.
Methods
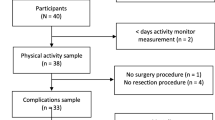
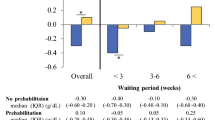
Patients who were scheduled to undergo open abdominal surgeries for HPB malignancies (major hepatectomy, pancreatoduodenectomy, or hepato-pancreatoduodenectomy) between 2016 and 2017 were included. The average steps per day were recorded by a pedometer and calculated for each patient during the preoperative waiting period. Physical activity levels were classified according to the average number of daily steps as poor (< 5000 steps/day) and good (≥ 5000 steps/day).
Results
Of the 105 eligible patients, 78 met the inclusion criteria. The median number of steps per day was 6174. There were 48 patients (62%) with good physical activity and 30 patients (38%) with poor physical activity. Patients with poor physical activity revealed a significantly higher rate of major complications with Clavien grade ≥ 3 (63% vs. 35%, p = 0.016), a higher rate of infectious complications (53% vs. 23%, p = 0.006), and a longer postoperative hospital stay (median, 30 vs. 21 days, p < 0.001) compared with those with good physical activity. After a multivariate analysis, poor physical activity was identified as an independent risk factor for the development of major complications (odds ratio, 2.842, p = 0.042) and infectious complications (odds ratio, 3.844, p = 0.007).
Conclusions
The current study demonstrated that preoperative physical activity levels are associated with the incidence of major postoperative complications following HPB surgery for malignancy.




Similar content being viewed by others
References
Simonsen C, de Heer P, Bjerre ED, et al. Sarcopenia and postoperative complication risk in gastrointestinal surgical oncology: a meta-analysis. Ann Surg. 2018;268:58–69.
Otsuji H, Yokoyama Y, Ebata T, et al. Preoperative sarcopenia negatively impacts postoperative outcomes following major hepatectomy with extrahepatic bile duct resection. World J Surg. 2015;39:1494–500.
Hayashi K, Yokoyama Y, Nakajima H, et al. Preoperative 6-minute walk distance accurately predicts postoperative complications after operations for hepato-pancreato-biliary cancer. Surgery. 2017;161:525–32.
Nakajima H, Yokoyama Y, Inoue T, et al. Clinical benefit of preoperative exercise and nutritional therapy for patients undergoing hepato-pancreato-biliary surgeries for malignancy. Ann Surg Oncol. 2019;26:264–72.
West MA, Wischmeyer PE, Grocott MPW. Prehabilitation and nutritional support to improve perioperative outcomes. Curr Anesthesiol Rep. 2017;7:340–9.
Silver JK, Baima J. Cancer prehabilitation: an opportunity to decrease treatment-related morbidity, increase cancer treatment options, and improve physical and psychological health outcomes. Am J Phys Med Rehabil. 2013;92:715–27.
Meyerhardt JA, Heseltine D, Niedzwiecki D, et al. Impact of physical activity on cancer recurrence and survival in patients with stage III colon cancer: findings from CALGB 89803. J Clin Oncol. 2006;24:3535–41.
Onerup A, Bock D, Borjesson M, et al. Is preoperative physical activity related to post-surgery recovery?-a cohort study of colorectal cancer patients. Int J Colorectal Dis. 2016;31:1131–40.
Nilsson H, Angeras U, Bock D, et al. Is preoperative physical activity related to post-surgery recovery? A cohort study of patients with breast cancer. BMJ Open. 2016;6:e007997.
Orsini N, Mantzoros CS, Wolk A. Association of physical activity with cancer incidence, mortality, and survival: a population-based study of men. Br J Cancer. 2008;98:1864–9.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Clavien PA, Strasberg SM. Severity grading of surgical complications. Ann Surg. 2009;250:197–8.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149:713–24.
Koch M, Garden OJ, Padbury R, et al. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149:680–8.
Bassi C, Dervenis C, Butturini G, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8–13.
Shrikhande SV, Sivasanker M, Vollmer CM, et al. Pancreatic anastomosis after pancreatoduodenectomy: a position statement by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2017;161:1221–34.
Tudor-Locke C, Craig CL, Thyfault JP, Spence JC. A step-defined sedentary lifestyle index: < 5000 steps/day. Appl Physiol Nutr Metab. 2013;38:100–14.
Roy LB, Edwards PA, Barr LH. The value of nutritional assessment in the surgical patient. JPEN J Parenter Enteral Nutr. 1985;9:170–2.
McMillan DC, Crozier JE, Canna K, et al. Evaluation of an inflammation-based prognostic score (GPS) in patients undergoing resection for colon and rectal cancer. Int J Colorectal Dis. 2007;22:881–6.
Ignacio de Ulibarri J, Gonzalez-Madrono A, de Villar NG, et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. 2005;20:38–45.
Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–81.
Dronkers JJ, Chorus AM, van Meeteren NL, Hopman-Rock M. The association of pre-operative physical fitness and physical activity with outcome after scheduled major abdominal surgery. Anaesthesia. 2013;68:67–73.
Feeney C, Reynolds JV, Hussey J. Preoperative physical activity levels and postoperative pulmonary complications post-esophagectomy. Dis Esophagus. 2011;24:489–94.
Tatematsu N, Park M, Tanaka E, et al. Association between physical activity and postoperative complications after esophagectomy for cancer: a prospective observational study. Asian Pac J Cancer Prev 2013;14:47–51.
Esteban PA, Hernandez N, Novoa NM, Varela G. Evaluating patients’ walking capacity during hospitalization for lung cancer resection. Interact Cardiovasc Thorac Surg. 2017;25:268–71.
Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71 Suppl 2:1–14.
Crouter SE, Schneider PL, Karabulut M, Bassett DR, Jr. Validity of 10 electronic pedometers for measuring steps, distance, and energy cost. Med Sci Sports Exerc. 2003;35:1455–60.
Schmidt T, van Mackelenbergh M, Wesch D, Mundhenke C. Physical activity influences the immune system of breast cancer patients. J Cancer Res Ther. 2017;13:392–8.
Hutnick NA, Williams NI, Kraemer WJ, et al. Exercise and lymphocyte activation following chemotherapy for breast cancer. Med Sci Sports Exerc. 2005;37:1827–35.
Sprod LK, Palesh OG, Janelsins MC, et al. Exercise, sleep quality, and mediators of sleep in breast and prostate cancer patients receiving radiation therapy. Community Oncol. 2010;7:463–71.
Tudor-Locke C, Bassett DR, Jr. How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med. 2004;34:1–8.
Schmidt MD, Cleland VJ, Shaw K, et al. Cardiometabolic risk in younger and older adults across an index of ambulatory activity. Am J Prev Med. 2009;37:278–84.
Sisson SB, Camhi SM, Church TS, et al. Accelerometer-determined steps/day and metabolic syndrome. Am J Prev Med. 2010;38:575–82.
McKercher CM, Schmidt MD, Sanderson KA, et al. Physical activity and depression in young adults. Am J Prev Med. 2009;36:161–4.
Grimmett C, Corbett T, Brunet J, et al. Systematic review and meta-analysis of maintenance of physical activity behaviour change in cancer survivors. Int J Behav Nutr Phys Act. 2019;16:37.
Kim HK, Suzuki T, Saito K, et al. Effects of exercise and amino acid supplementation on body composition and physical function in community-dwelling elderly Japanese sarcopenic women: a randomized controlled trial. J Am Geriatr Soc. 2012;60:16–23.
Acknowledgment
This work was supported in part by a Grant (No. H29-B31 to H. Nakajima) from the Japanese Physical Therapy Association. The authors sincerely thank all of the patients, collaborating physicians, and other medical staff for their important contributions to this study.
Disclosure
The authors affirm that they have no financial or personal affiliations (including research funding) or other involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Fig.
1 Leaflet used for guiding patients. Supplementary Fig. 2 Correlation plots for physical activity and preoperative serum albumin (DOCX 252 kb)
Rights and permissions
About this article
Cite this article
Nakajima, H., Yokoyama, Y., Inoue, T. et al. How Many Steps Per Day are Necessary to Prevent Postoperative Complications Following Hepato-Pancreato-Biliary Surgeries for Malignancy?. Ann Surg Oncol 27, 1387–1397 (2020). https://doi.org/10.1245/s10434-020-08218-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08218-x