Abstract
Background
Patients with esophageal cancer have poor overall survival, with positive resection margins worsening survival. Margin positivity rates are used as quality measures in other malignancies, but modifiable risk factors are necessary to develop actionable targets for improvement. Our objectives were to (1) evaluate trends in esophageal cancer margin positivity, and (2) identify modifiable patient/hospital factors associated with margin positivity.
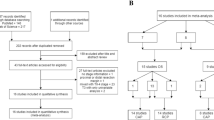
Methods
Patients who underwent esophagectomy from 2004 to 2015 were identified from the National Cancer Database. Trends in margin positivity by time and hospital volume were evaluated using Cochrane–Armitage tests. Associations between patient/hospital factors and margin positivity were assessed by multivariable logistic regression.
Results
Among 29,706 patients who underwent esophagectomy for cancer, 9.37% had positive margins. Margin positivity rates decreased over time (10.62% in 2004 to 8.61% in 2015; p < 0.001). Older patients (≥ 75 years) were more likely to have positive margins [odds ratio (OR) 2.04, 95% confidence interval (CI) 1.42–2.92], as were patients with a Charlson–Deyo Index ≥ 3 (OR 1.84, 95% CI 1.08–3.12). Patients who received neoadjuvant therapy were less likely to have positive margins (OR 0.37, 95% CI 0.29–0.47), while laparoscopic surgical approach was associated with increased margin positivity (OR 1.70, 95% CI 1.40–2.06). As the hospital annual esophagectomy volume increased, margin positivity rates decreased (7.76% in the fourth quartile vs. 11.39% in the first quartile; OR 0.70, 95% CI 0.49–0.99).
Conclusions
Use of neoadjuvant therapy, surgical approach, and hospital volume are modifiable risk factors for margin positivity in esophageal cancer. These factors should be considered in treatment planning, and margin positivity rates could be considered as a quality measure in esophageal cancer.


Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34.
Portale G, Hagen JA, Peters JH, et al. Modern 5-year survival of resectable esophageal adenocarcinoma: single institution experience with 263 patients. J Am Coll Surg. 2006;202(4):588–96.
Ajani JA, D’Amico TA, Bentrem DJ, et al. Esophageal and esophagogastric junction cancers, Version 2.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019;17(7):855–83.
Markar SR, Gronnier C, Duhamel A, et al. Significance of microscopically incomplete resection margin after esophagectomy for esophageal cancer. Ann Surg. 2016;263(7):712–18.
Gilbert S, Martel AB, Seely AJ, et al. Prognostic significance of a positive radial margin after esophageal cancer resection. J Thorac Cardiovasc Surg. 2015;149(2):548–55.
Hulshoff JB, Faiz Z, Karrenbeld A, et al. Prognostic value of the circumferential resection margin in esophageal cancer patients after neoadjuvant chemoradiotherapy. Ann Surg Oncol. 2015;22 Suppl 3:S1301–S1309.
Wu J, Chen QX, Teng LS, Krasna MJ. Prognostic significance of positive circumferential resection margin in esophageal cancer: a systematic review and meta-analysis. Ann Thorac Surg. 2014;97(2):446–53.
Nagtegaal ID, Quirke P. What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol. 2008;26(2):303–12.
Dietz DW, Consortium for optimizing surgical treatment of rectal cancer. Multidisciplinary management of rectal cancer: the OSTRICH. J Gastrointest Surg. 2013;17(10):1863–868.
Rickles AS, Dietz DW, Chang GJ, et al. High rate of positive circumferential resection margins following rectal cancer surgery: a call to action. Ann Surg. 2015;262(6):891–98.
van der Werf LR, Cords C, Arntz I, et al. Population-based study on risk factors for tumor-positive resection margins in patients with gastric cancer. Ann Surg Oncol. 2019;26(7):2222–233.
Schwarz RE. Clinical trends and effects on quality metrics for surgical gastroesophageal cancer care. Transl Gastroenterol Hepatol. 2018;19(3):43.
Samson P, Puri V, Broderick S, Patterson GA, Meyers B, Crabtree T. Adhering to quality measures in esophagectomy is associated with improved survival in all stages of esophageal cancer. Ann Thorac Surg. 2017;103(4):1101–108.
Steele GDJ, Winchester DP, Menck HR. The national cancer data base. A mechanism for assessment of patient care. Cancer. 1994;73(2):499–04.
Boffa DJ, Rosen JE, Mallin K, et al. Using the national cancer database for outcomes research: a review. JAMA Oncol. 2017;3(12):1722–728.
Mallin K, Browner A, Palis B, et al. Incident cases captured in the national cancer database compared with those in U.S. population based central cancer registries in 2012–2014. Ann Surg Oncol. 2019;26(6):1604–612.
Winchester DP, Stewart AK, Phillips JL, Ward EE. The national cancer data base: past, present, and future. Ann Surg Oncol. 2010;17(1):4–7.
Merkow RP, Hall BL, Cohen ME, et al. Relevance of the c-statistic when evaluating risk-adjustment models in surgery. J Am Coll Surg. 2012;214(5):822–39.
Steyerberg EW, Vickers AJ, Cook NR, et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology. 2010;21(1):128–38.
Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med. 2010;29(9):1037–057.
Adam MA, Thomas S, Youngwirth L, et al. Is there a minimum number of thyroidectomies a surgeon should perform to optimize patient outcomes? Ann Surg. 2017;265(2):402–07.
van Hagen P, Hulshof MC, van Lanschott JJ, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366(22):2074–2084.
Mariette C, Fabre S, Balon JM, Finzi L, Triboulet JP. Factors predictive of complete resection of operable esophageal cancer: review of 746 patients. Gastroenterol Clin Biol. 2002;26(5):454–62.
Walsh TN, Noonan N, Hollywood D, Kelly A, Keeling N, Hennessy TP. A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med. 1996;335(7):426–27.
Tepper J, Krasna MJ, Niedziecki D, et al. Phase III trial of trimodality therapy with cisplatin, fluorouracil, radiotherapy, and surgery compared with surgery alone for esophageal cancer: CALGB 9781. J Clin Oncol. 2008;26(7):1086–092.
Brown LM, Hoover R, Silverman D, et al. Excess incidence of squamous cell esophageal cancer among US Black men: role of social class and other risk factors. Am J Epidemiol. 2001;132(2):114–22.
Wang N, Cao F, Liu F, et al. The effect of socioeconomic status on health-care delay and treatment of esophageal cancer. J Transl Med. 2015;24(13):241.
Jang BS, Chang JH. Socioeconomic status and survival outcomes in elderly cancer patients: a national health insurance service-elderly sample cohort study. Cancer Med. 2019;8(7):3604–613.
Revels SL, Morris AM, Reddy RM, Akateh C, Wong SL. Racial disparities in esophageal cancer outcomes. Ann Surg Oncol. 2013;20(4):1136–141.
Orosco RK, Tapia VJ, Califano JA, et al. Positive surgical margins in the 10 most common solid cancers. Sci Rep. 2018;8(1):5686.
Wen J, Linghu EQ, Yang YS, Liu QS, Yang J, Lu ZS. Associated risk factor analysis for positive resection margins after endoscopic submucosal dissection in early-stage gastric cancer. J BUON. 2015;20(2):421–27.
Ichikawa H, Kosugi SI, Kanda T, et al. Surgical and long-term outcomes following oesophagectomy in oesophageal cancer patients with comorbidity. Int J Surg. 2016;36(Pt A):212–18.
Merkow RP, Bilimoria KY, McCarter MD, Chow WB, Ko CY, Bentrem DJ. Use of multimodality neoadjuvant therapy for esophageal cancer in the United States: assessment of 987 hospitals. Ann Surg Oncol. 2012;19(2):357–64.
Barbour AP, Rizk NP, Gonen M, et al. Adenocarcinoma of the gastroesophageal junction: infludence of esophageal resection margin and operative approach on outcome. Ann Surg. 2007;246(1):1–8.
Foley KG, Christian A, Patel N, Lewis WG, Roberts SA. Radiological prediction of positive circumferential resection margin in oesophageal cancer. Eur J Radiol. 2018;107:119–24.
Medical Research Council Oesophageal Cancer Working Group. Surgical resection with or without preoperative chemotherapy in oesophageal cancer: a randomised controlled trial. Lancet. 2002;359(9319):1727–733.
Shah RD, Cassano AD, Neifeld JP. Neoadjuvant therapy for esophageal cancer. World J Gastrointest Oncol. 2014;5(10):403–06.
Rodriguez-Sanjuan JC, Gomez-Ruiz M, Trugeda-Carrera S, Manuel-Palazuelos C, Lpez-Useros A, Gomez-Fleitas M. Laparoscopic and robotic-assisted laparoscopic digestive surgery: present and future directions. World J Gastroenterol. 2016;22(6):1975–004.
Tsujimoto H, Takahata R, Nomura S, et al. Video-assisted thoracoscopic surgery for esophageal cancer attenuates postoperative systemic reponses and pulmonary complications. Surgery. 2012;151(5):667–73.
Hanna GB, Arya S, Markar SR. Variation in the standard of minimally invasive esophagectomy for cancer—systematic review. Semin Thorac Cardiovasc Surg. 2012;24(3):176–87.
Biere SS, van Berge Henegouwen MI, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label randomised controlled trial. Lancet. 2012;379(9829):1887–892.
Uttley L, Campbell F, Rhodes M, Cantrell A, Stegenga H, Lloyd-Jones M. Minimally invasive oesophagectomy versus open surgery: is there an advantage? Surg Endosc. 2013;27(3):724–31.
Panni RZ, Guerra J, Hawkins WG, Hall BL, Asbun HJ, Sanford DE. National pancreatic fistula rates after minimally invasive pancreaticoduodenectomy: a NSQIP analysis. J Am Coll Surg. 2019;229(2):192–99.
Wei D, Johnston S, Goldstein L, Nagle D. Minimally invasive colectomy is associated with reduced risk of anastomotic leak and other major perioperative complications and reduced hospital resource utilization as compared with open surgery: a retrospective population-based study of comparative effectiveness and trends of surgical approach. Surg Endosc. 2019; https://doi.org/10.1007/s00464-019-06805-y.
Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364(22):2128–137.
Markar SR, Karthikesalingam A, Thrumurthy S, Low DE. Volume-outcome relationship in surgery for esophageal malignancy: systematic review and meta-analysis 2000-2011. J Gastrointest Surg. 2012;16(5):1055–063.
Casson AG, van Lanschott JJ. Improving outcomes after esophagectomy: the impact of operative volume. J Surg Oncol. 2005;92(3):262–66.
The Leapfrog Group Surgical Volume. Available at: https://www.leapfroggroup.org/ratings-reports/surgical-volume. Accessed June 2019.
Christian CK, Gustafson ML, Betensky RA, Daley J, Znner MJ. The Leapfrog volume criteria may fall short in identifying high-quality surgical centers. Ann Surg. 2003;238(4):447–55.
Varghese TKJ, Wood DE, Farjah F, et al. Variation in esophagectomy outcomes in hospitals meeting Leapfrog volume outcome standards. Ann Thorac Surg. 2011;91(4):1003–009.
Funding
This study was supported by the Northwestern Institute for Comparative Effectiveness Research in Oncology (NICER-Onc) of the Robert H. Lurie Comprehensive Cancer Center. RK is supported by a postdoctoral research fellowship from the National Heart, Lung, and Blood Institute (5T32HL094293); DDO is supported by the National Cancer Institute (K07CA216330); RPM is supported by the Agency for Healthcare Research and Quality (K12HS026385) and an Institutional Research Grant from the American Cancer Society (IRG-18-163-24); and DJB is supported by a Veteran’s Administration Merit Award (I01HX002290).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Cary Jo R. Schlick, Rhami Khorfan, David D. Odell, Ryan P. Merkow, and David J. Bentrem report no conflicts of interest, financial or otherwise, related to this work. The NCDB is a joint project of the CoC of the American College of Surgeons and the American Cancer Society. The CoC’s NCDB and the hospitals participating in the CoC NCDB are the source of the de-identified data used herein. They have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schlick, C.J.R., Khorfan, R., Odell, D.D. et al. Margin Positivity in Resectable Esophageal Cancer: Are there Modifiable Risk Factors?. Ann Surg Oncol 27, 1496–1507 (2020). https://doi.org/10.1245/s10434-019-08176-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-08176-z