Abstract
Background
Esophageal neuroendocrine tumors (eNETs) are exceedingly rare, aggressive and have a poor prognosis. Treatment guidelines are ill-defined and mainly based on evidence from case reports and analogous experiences drawn from similar disease sites.
Methods
The NCDB was reviewed for histologically confirmed stage I–III, primary eNETs from 2006 to 2014. Patients were grouped into whether or not they underwent primary tumor resection. Univariate, multivariable, and full bipartite propensity score (PS) adjusted Cox regression analyses were used to assess overall and relative survival differences.
Results
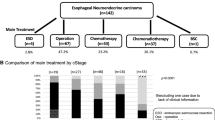
A total of 250 patients were identified. Mean age was 65.0 (standard deviation [SD] 11.9) years, and 174 (69.6%) patients were male. Most patients had stage III disease (n = 136, 54.4%), and the most common type of NET was small cell eNET (n = 111, 44.4%). Chemotherapy was used in 186 (74.4%), radiation therapy in 178 (71.2%), and oncological resection was performed in 69 (27.6%) patients. Crude 2-year survival rates were higher in the operated (57.3%) compared with the nonoperated group (35.2%; p < 0.001). The survival benefit held true after multivariable adjustment (hazard ratio [HR] 0.47, 95% confidence interval [CI] 0.32–0.69, p < 0.001). After full bipartite PS adjustment analysis, survival was longer for patients who received a surgical resection compared with those who did not (HR 0.48, 95% CI 0.31–0.75, p = 0.003) with a corresponding 2-year overall survival rate of 63.3% (95% CI 52.0–77.2) versus 38.8% (95% CI 30.9–48.8), respectively.
Conclusions
Multimodal treatment that includes surgery is associated with better overall survival for eNETs. Additional research is needed to more definitively identify patients who benefit from esophagectomy and to establish an appropriate treatment algorithm.

Similar content being viewed by others
References
Ilett E, Langer S, Olsen I, Federspiel B, Kjær A. Neuroendocrine carcinomas of the gastroenteropancreatic system: a comprehensive review. Diagnostics. 2015. http://www.mdpi.com/2075-4418/5/2/119/htm. Accessed 28 Aug 2017.
Estrozi B, Bacchi CE. Neuroendocrine tumors involving the gastroenteropancreatic tract: a clinicopathological evaluation of 773 cases. Clinics (Sao Paulo). 2011;66(10):1671–5. https://doi.org/10.1590/s1807-59322011001000002.
Deng H, Ni P, Wang Y, Wang W. Neuroendocrine carcinoma of the esophagus: clinical characteristics and prognostic evaluation of 49 cases with surgical resection. J Thorac. 2016. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4886019/. Accessed 28 Aug 2017.
Lee C, Lim Y, Park S, Jang B. The clinical features and treatment modality of esophageal neuroendocrine tumors: a multicenter study in Korea. BMC. 2014. https://bmccancer.biomedcentral.com/articles/10.1186/1471-2407-14-569. Accessed 28 Aug 2017.
Schizas D, Mastoraki A, Kirkilesis GI, et al. Neuroendocrine tumors of the esophagus: state of the art in diagnostic and therapeutic management. J Gastrointest Cancer. 2017;48(4):299–304. https://doi.org/10.1007/s12029-017-9978-x.
Chin JL, O’Toole D. Diagnosis and management of upper gastrointestinal neuroendocrine tumors. Clin Endosc. 2017;50(6):520–9. https://doi.org/10.5946/ce.2017.181.
Egashira A, Morita M, Kumagai R, et al. Neuroendocrine carcinoma of the esophagus: Clinicopathological and immunohistochemical features of 14 cases. PLoS One. 2017;12(3):e0173501. https://doi.org/10.1371/journal.pone.0173501.
Caplin ME, Baudin E, Ferolla P, et al. Pulmonary neuroendocrine (carcinoid) tumors: European Neuroendocrine Tumor Society expert consensus and recommendations for best practice for typical and atypical pulmonary carcinoids. Ann Oncol. 2015;26(8):1604–20. https://doi.org/10.1093/annonc/mdv041.
Kuo C, Hsieh C, Chan M, Li A. Small cell carcinoma of the esophagus: a report of 16 cases from a single institution and literature review. Ann Thorac. 2011. http://www.sciencedirect.com/science/article/pii/S0003497510021089. Accessed 28 Aug 2017.
Hou X, Wei J-C, Wu J-X, et al. Multidisciplinary Modalities achieve encouraging long-term survival in resectable limited-disease esophageal small cell carcinoma. Ganti AK, editor. PLoS One. 2013;8(7):e69259. https://doi.org/10.1371/journal.pone.0069259.
Nemoto K, Zhao H-J, Goto T, et al. Radiation therapy for limited-stage small-cell esophageal cancer. Am J Clin Oncol. 2002;25(4):404–7. http://www.ncbi.nlm.nih.gov/pubmed/12151974. Accessed 26 Oct 2018.
Saddoughi SA, Taswell J, Harmsen WS, et al. Surgical resection of rare esophageal cancers. Ann Thorac Surg. 2016;101:311–5. https://doi.org/10.1016/j.athoracsur.2015.06.015.
Chen W-W, Wang F, Chen S, et al. Detailed analysis of prognostic factors in primary esophageal small cell carcinoma. Ann Thorac Surg. 2014;97(6):1975–81. https://doi.org/10.1016/j.athoracsur.2014.02.037.
Rindi G, Wiedenmann B. Neuroendocrine neoplasms of the gut and pancreas: new insights. Nat Rev Endocrinol. 2012;8(1):54–64. https://doi.org/10.1038/nrendo.2011.120.
Luketich JD, Pennathur A, Awais O, et al. Outcomes after minimally invasive esophagectomy: review of over 1000 patients. Ann Surg. 2012;256(1):95–103. https://doi.org/10.1097/sla.0b013e3182590603.
Hu Y, Mcmurry TL, Stukenborg GJ, Kozower BD. Readmission predicts 90-day mortality after esophagectomy: Analysis of Surveillance, Epidemiology, and End Results Registry linked to Medicare outcomes. J Thorac Cardiovasc Surg. 2015;150:1254–60. https://doi.org/10.1016/j.jtcvs.2015.08.071.
Soriano TT, Eslick G, Vanniasinkam T. Long-term nutritional outcome and health related quality of life of patients following esophageal cancer surgery: a meta-analysis. Nutr Cancer. 2017:1–12. https://doi.org/10.1080/01635581.2018.1412471.
Brenner B, Tang LH, Klimstra DS, Kelsen DP. Small-cell carcinomas of the gastrointestinal tract: a review. J Clin Oncol. 2004;22(13):2730–9. https://doi.org/10.1200/jco.2004.09.075.
Hansen BB, Klopfer SO. Optimal full matching and related designs via network flows. J Comput Graph Stat. 2006;15(3):609–27. https://doi.org/10.1198/106186006x137047.
Ho DE, Imai K, King G, Stuart EA. MatchIt: Nonparametric Preprocessing for Parametric Causal Inference. Vol. 42; 2011. http://www.jstatsoft.org/. Accessed 26 Oct 2018.
Baiocchi M, Small DS, Yang L, Polsky D, Groeneveld PW. Near/far matching: a study design approach to instrumental variables. Heal Serv Outcomes Res Methodol. 2012;12(4):237–53. https://doi.org/10.1007/s10742-012-0091-0.
Angrist JD, Imbens GW, Rubin DB. Identification of causal effects using instrumental variables. J Am Stat Assoc. 1996;91(434):444–55. https://doi.org/10.1080/01621459.1996.10476902.
Series PH-ERR, 1988 undefined. Causal inference, path analysis and recursive structural equations models. Wiley Online Libr. http://onlinelibrary.wiley.com/doi/10.1002/j.2330-8516.1988.tb00270.x/full. Accessed 18 Feb 2018.
Pohar M, Stare J. Making relative survival analysis relatively easy. Comput Biol Med. 2007;37(12):1741–9. https://doi.org/10.1016/j.compbiomed.2007.04.010.
Situ D, Lin Y, Long H, et al. Surgical treatment for limited-stage primary small cell cancer of the esophagus. Ann Thorac Surg. 2013;95(3):1057–62. https://doi.org/10.1016/j.athoracsur.2012.11.014.
Funakoshi S, Hashiguchi A, Teramoto K, et al. Second-line chemotherapy for refractory small cell neuroendocrine carcinoma of the esophagus that relapsed after complete remission with irinotecan plus cisplatin therapy: case report and review of the literature. Oncol Lett. 2013;5(1):117–22. https://doi.org/10.3892/ol.2012.1008.
Klöppel G. Classification and pathology of gastroenteropancreatic neuroendocrine neoplasms. Endocr Relat Cancer. 2011;18(S1):S1–16. https://doi.org/10.1530/erc-11-0013.
Kuo CH, Hsieh CC, Chan ML, et al. Small cell carcinoma of the esophagus: a report of 16 cases from a single institution and literature review. Ann Thorac Surg. 2011. http://dx.doi.org/10.1016/j.athoracsur.2010.09.030.
Tanaka T, Matono S, Nagano T, et al. Original article: Surgical management for small cell carcinoma of the esophagus. Dis Esophagus. 2010;23(6):502–5. https://doi.org/10.1111/j.1442-2050.2009.01045.x.
Alese OB, Jiang R, Shaib W, et al. High-Grade Gastrointestinal Neuroendocrine Carcinoma Management and Outcomes: A National Cancer Database Study. Oncologist. November 2018:theoncologist.2018-0382. https://doi.org/10.1634/theoncologist.2018-0382.
Chen S, Yang J, Yang W, Weng H. Treatment and prognosis of limited disease primary small cell carcinoma of esophagus. Dis. 2011. https://academic.oup.com/dote/article-abstract/24/2/114/2328443. Accessed 21 Sept 2017.
Yau KK, Siu WT, Wong DCT, et al. Non-operative management of small cell carcinoma of esophagus. Dis Esophagus. 2007;20(6):487–90. https://doi.org/10.1111/j.1442-2050.2007.00635.x.
Dhungel B, Diggs BS, Hunter JG, Sheppard BC, Vetto JT, Dolan JP. Patient and peri-operative predictors of morbidity and mortality after esophagectomy: American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP), 2005-2008. J Gastrointest Surg. 2010;14(10):1492–501. https://doi.org/10.1007/s11605-010-1328-2.
Gurien LA, Tepas JJ, Lind DS, et al. How Safe Is the Safety Net? Comparison of Ivor-Lewis Esophagectomy at a Safety-Net Hospital Using the NSQIP Database. J Am Coll Surg. 2018;226(4):680–4. https://doi.org/10.1016/j.jamcollsurg.2017.12.036.
Zhang C, Wu Q-C, Hou P-Y, et al. Impact of the method of reconstruction after oncologic oesophagectomy on quality of life — a prospective, randomised study. Eur J Cardio-Thoracic Surg. 2010;39:109–14. https://doi.org/10.1016/j.ejcts.2010.04.032.
Hsu P-K, Chen H-S, Wu S-C, et al. Impact of hospital volume on long-term survival after resection for oesophageal cancer: a population-based study in Taiwan†. Eur J Cardio-Thoracic Surg. 2014;46(6):e127–35. https://doi.org/10.1093/ejcts/ezu377.
Dikken JL, van Sandick JW, Allum WH, et al. Differences in outcomes of oesophageal and gastric cancer surgery across Europe. Br J Surg. 2013;100(1):83–94. https://doi.org/10.1002/bjs.8966.
Munasinghe A, Markar SR, Mamidanna R, et al. Is it time to centralize high-risk cancer care in the united states? comparison of outcomes of esophagectomy between England and the United States. Ann Surg. 2015;262(1):79–85. https://doi.org/10.1097/sla.0000000000000805.
Acknowledgment
The authors thank the American College of Surgeons and the American Cancer Society for providing patient information through the NCDB used for this investigation. Furthermore, we thank the patients whose information through the NCDB allowed us to perform the investigation for this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The author declares that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Erdem, S., Troxler, E., Warschkow, R. et al. Is There a Role for Surgery in Patients with Neuroendocrine Tumors of the Esophagus? A Contemporary View from the NCDB. Ann Surg Oncol 27, 671–680 (2020). https://doi.org/10.1245/s10434-019-07847-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07847-1