Abstract
Background
Dogmatic denial of vasopressor agents for blood pressure regulation during free-flap surgery is associated with concomitant large-volume intraoperative fluid administration. Yet, the doctrinal banning of vasopressors during microvascular breast reconstruction still is a subject of controversy. Several retrospective observations have recently drawn attention to serious iatrogenic consequences of intravenous crystalloid overload in microsurgery such as thrombus formation and increased flap failure rates.
Methods
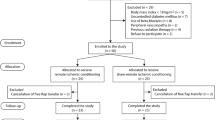
This prospective randomized controlled trial investigated the potential effects of fluid-restrictive vasopressor-dominated hemodynamic support (FRV) compared with vasopressor-restrictive liberal fluid administration (LFA) on clinically relevant perfusion of the deep inferior epigastric perforator (DIEP) flap via intraoperative indocyanine green (ICG) fluorescence imaging. The primary end point of the study was quantitative assessment of the percentage of insufficiently perfused tissue (NP) on the overall flap. Major complications were assessed as secondary end points.
Results
In 44 DIEP flap breast reconstructions after mastectomy, FRV circulatory support resulted in no statistically significant difference in total flap perfusion as detected via ICG fluorescence imaging in direct comparison with a traditional LFA strategy (NPFRV, 31.8% ± 12.2% vs NPLFA, 29.5% ± 13.3%; p = 0.559). One flap failure was registered with LFA, whereas no major complication occurred in the FRV cohort.
Conclusions
According to the results of this study, neither a norepinephrine concentration of 0.065 ± 0.020 μg/kg/min (FRV) nor fluid administration of 5.1 ± 2.2 ml/kg/h (LFA) has a clinically significant impact on microperfusion in a standard DIEP flap procedure for breast reconstruction. Consistent with the current literature reporting a rise in complications with intraoperative fluid over-resuscitation, one flap failure occurred in the LFA cohort.




Similar content being viewed by others
References
Sigurdsson GH, Thomson D. Anaesthesia and microvascular surgery: clinical practice and research. Eur J Anaesthesiol. 1995;12:101–22.
Hagau N, Longrois D. Anesthesia for free vascularized tissue transfer. Microsurgery. 2009;29:161–7.
Massey MF, Gupta DK. The effects of systemic phenylephrine and epinephrine on pedicle artery and microvascular perfusion in a pig model of myoadipocutaneous rotational flaps. Plast Reconstr Surg. 2007;120:1289–99.
Szabo Eltorai A, Huang CC, Lu JT, Ogura A, Caterson SA, Orgill DP. Selective intraoperative vasopressor use is not associated with increased risk of DIEP flap complications. Plast Reconstr Surg. 2017;140:70e–7e.
Hong JPJ, Suh HSP. Discussion: selective intraoperative vasopressor use is not associated with increased risk of DIEP flap complications. Plast Reconstr Surg. 2017;140:78e–9e.
Ibrahim AM, Kim PS, Rabie AN, Lee BT, Lin SJ. Vasopressors and reconstructive flap perfusion: a review of the literature comparing the effects of various pharmacologic agents. Ann Plast Surg. 2014;73:245–8.
Pattani KM, Byrne P, Boahene K, Richmon J. What makes a good flap go bad? A critical analysis of the literature of intraoperative factors related to free flap failure. Laryngoscope. 2010;120:717–23.
Chen C, Nguyen MD, Bar-Meir E, et al. Effects of vasopressor administration on the outcomes of microsurgical breast reconstruction. Ann Plast Surg. 2010;65:28–31.
Zhong T, Neinstein R, Massey C, et al. Intravenous fluid infusion rate in microsurgical breast reconstruction: important lessons learned from 354 free flaps. Plast Reconstr Surg. 2011;128:1153–60.
Motakef S, Mountziaris PM, Ismail IK, Agag RL, Patel A. Emerging paradigms in perioperative management for microsurgical free tissue transfer: review of the literature and evidence-based guidelines. Plast Reconstr Surg. 2015;135:290–9.
Haughey BH, Wilson E, Kluwe L, et al. Free flap reconstruction of the head and neck: analysis of 241 cases. Otolaryngol Head Neck Surg. 2001;125:10–17.
Clark JR, McCluskey SA, Hall F, et al. Predictors of morbidity following free-flap reconstruction for cancer of the head and neck. Head Neck. 2007;29:1090–101.
Corcoran T, Rhodes JE, Clarke S, Myles PS, Ho KM. Perioperative fluid management strategies in major surgery: a stratified meta-analysis. Anesth Analg. 2012;114:640–51.
Nisanevich V, Felsenstein I, Almogy G, Weissman C, Einav S, Matot I. Effect of intraoperative fluid management on outcome after intraabdominal surgery. Anesthesiology. 2005;103:25–32.
Brandstrup B, Tonnesen H, Beier-Holgersen R, et al. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg. 2003;238:641–8.
Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg. 1994;32:32–8.
Anker AM, Prantl L, Strauss C, et al. Vasopressor support vs liberal fluid administration in deep inferior epigastric perforator (DIEP) free-flap breast reconstruction: a randomized controlled trial. Clin Hemorheol Microcirc. 2018;69:37–44.
Holm C, Mayr M, Hofter E, Ninkovic M. Perfusion zones of the DIEP flap revisited: a clinical study. Plast Reconstr Surg. 2006;117:37–43.
Giunta RE, Holzbach T, Taskov C, et al. Prediction of flap necrosis with laser induced indocyanine green fluorescence in a rat model. Br J Plast Surg. 2005;58:695–701.
Moyer HR, Losken A. Predicting mastectomy skin flap necrosis with indocyanine green angiography: the gray area defined. Plast Reconstr Surg. 2012;129:1043–8.
Temple-Oberle C, Shea-Budgell MA, Tan M, et al. Consensus review of optimal perioperative care in breast reconstruction: enhanced recovery after surgery (ERAS) society recommendations. Plast Reconstr Surg. 2017;139:1056e–71e.
Wong C, Saint-Cyr M, Mojallal A, et al. Perforasomes of the DIEP flap: vascular anatomy of the lateral versus medial row perforators and clinical implications. Plast Reconstr Surg. 2010;125:772–82.
Diep GK, Hui JY, Marmor S, et al. Postmastectomy reconstruction outcomes after intraoperative evaluation with indocyanine green angiography versus clinical assessment. Ann Surg Oncol. 2016;23:4080–5.
Wang WZ, Anderson G, Firrell JC. Arteriole constriction following ischemia in denervated skeletal muscle. J Reconstr Microsurg. 1995;11:99–106.
Lorenzetti F, Suominen S, Tukiainen E, et al. Evaluation of blood flow in free microvascular flaps. J Reconstr Microsurg. 2001;17:163–7.
Eley KA, Young JD, Watt-Smith SR. Power spectral analysis of the effects of epinephrine, norepinephrine, dobutamine, and dopexamine on microcirculation following free tissue transfer. Microsurgery. 2013;33:275–81.
Eley KA, Young JD, Watt-Smith SR. Epinephrine, norepinephrine, dobutamine, and dopexamine effects on free-flap skin blood flow. Plast Reconstr Surg. 2012;130:564–70.
Kelly DA, Reynolds M, Crantford C, Pestana IA. Impact of intraoperative vasopressor use in free tissue transfer for head, neck, and extremity reconstruction. Ann Plast Surg. 2014;72:S135–8.
Harris L, Goldstein D, Hofer S, Gilbert R. Impact of vasopressors on outcomes in head and neck free tissue transfer. Microsurgery. 2012;32:15–9.
Feldheiser A, Aziz O, Baldini G, et al. Enhanced recovery after surgery (ERAS) for gastrointestinal surgery, part 2: consensus statement for anaesthesia practice. Acta Anaesthesiol Scand. 2016;60:289–334.
Hendrix RJ, Damle A, Williams C, et al. Restrictive intraoperative fluid therapy is associated with decreased morbidity and length of stay following hyperthermic intraperitoneal chemoperfusion. Ann Surg Oncol. 2019;26:490–6.
Ettinger KS, Arce K, Lohse CM, et al. Higher perioperative fluid administration is associated with increased rates of complications following head and neck microvascular reconstruction with fibular free flaps. Microsurgery. 2017;37:128–36.
Patel RS, McCluskey SA, Goldstein DP, et al. Clinicopathologic and therapeutic risk factors for perioperative complications and prolonged hospital stay in free-flap reconstruction of the head and neck. Head Neck. 2010;32:1345–53.
Fang L, Liu J, Yu C, Hanasono MM, Zheng G, Yu P. Intraoperative use of vasopressors does not increase the risk of free-flap compromise and failure in cancer patients. Ann Surg. 2018;268:379–84.
Wade RG, Razzano S, Sassoon EM, Haywood RM, Ali RS, Figus A. Complications in DIEP flap breast reconstruction after mastectomy for breast cancer: a prospective cohort study comparing unilateral versus bilateral reconstructions. Ann Surg Oncol. 2017;24:1465–74.
Pashikanti L, Von Ah D. Impact of early mobilization protocol on the medical-surgical inpatient population: an integrated review of literature. Clin Nurse Spec. 2012;26:87–94.
Gocze I, Jauch D, Gotz M, et al. Biomarker-guided intervention to prevent acute kidney injury after major surgery: the prospective randomized BigpAK study. Ann Surg. 2018;267:1013–20.
Perazella MA. Onco-nephrology: renal toxicities of chemotherapeutic agents. Clin J Am Soc Nephrol. 2012;7:1713–21.
Succar L, Pianta TJ, Davidson T, Pickering JW, Endre ZH. Subclinical chronic kidney disease modifies the diagnosis of experimental acute kidney injury. Kidney Int. 2017;92:680–92.
Futier E, Lefrant JY, Guinot PG, et al. Effect of individualized vs standard blood pressure management strategies on postoperative organ dysfunction among high-risk patients undergoing major surgery: a randomized clinical trial. JAMA. 2017;318:1346–57.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MP4 1009 kb)
Rights and permissions
About this article
Cite this article
Anker, A.M., Prantl, L., Strauss, C. et al. Assessment of DIEP Flap Perfusion with Intraoperative Indocyanine Green Fluorescence Imaging in Vasopressor-Dominated Hemodynamic Support Versus Liberal Fluid Administration: A Randomized Controlled Trial With Breast Cancer Patients. Ann Surg Oncol 27, 399–406 (2020). https://doi.org/10.1245/s10434-019-07758-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07758-1