Abstract
Background
Locoregional recurrence (LRR) after breast-conserving surgery (BCS) for ductal carcinoma in situ (DCIS) is increased in young women. We examined the impact of age on LRR and distant disease after mastectomy for DCIS ± microinvasion.
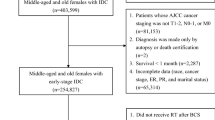
Methods
We identified consecutive patients with DCIS ± microinvasion treated with mastectomy from 1995 to 2017. LRR was defined as recurrence at the ipsilateral chest wall or regional nodes.
Results
Overall, 3121 cases were identified, of which 421 (13.5%) had DCIS + microinvasion. Median age was 49 years and median follow-up was 6.4 years; 821 were followed for 10 or more years. Thirty-four LRRs were observed: 33 (97%) were invasive, and 23 (68%) were in the chest wall alone. Cumulative 10-year LRR incidence was 1.4%. Age < 50 years, high grade, and DCIS + microinvasion were associated with LRR (p ≤ 0.001); however, margin status was not (p = 0.14). Adjusting for grade and DCIS + microinvasion, age < 50 years (hazard ratio [HR] 14.7, 95% confidence interval [CI] 3.5–61.5; p < 0.001) was associated with LRR. Compared with women ≥ 50 years of age, women age < 40 years had the highest risk (HR 27.0, 95% CI 6.0–121), and women age 40–49 years had intermediate risk (HR 11.8, 95% CI 2.8–50.5). The cumulative 10-year LRR incidence was 4.2% for women < 40 years of age, 2.0% for women 40–49 years of age, and 0.2% for women ≥ 50 years of age. Women age < 40 years had a 10-year distant disease rate of 1.6% versus women age 40–49 years (0.7%) and women age ≥ 50 years (0.7%) (log-rank p = 0.051). Grade, DCIS + microinvasion, and margins were unassociated with distant disease.
Conclusions
LRR after mastectomy for DCIS ± microinvasion is uncommon, but is more frequent among women < 50 years of age, particularly in those < 40 years of age. The 10-year LRR rate in this youngest group remains low at 4.2%. Young age is an independent risk factor for LRR after BCS or mastectomy.



Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7–30.
Narod SA, Iqbal J, Giannakeas V, Sopik V, Sun P. Breast cancer mortality after a diagnosis of ductal carcinoma in situ. JAMA Oncol. 2015;1(7):888–896.
Warnberg F, Garmo H, Emdin S, et al. Effect of radiotherapy after breast-conserving surgery for ductal carcinoma in situ: 20 years follow-up in the randomized SweDCIS Trial. J Clin Oncol. 2014;32(32):3613–3618.
Correa C, McGale P, Taylor C, et al. Overview of the randomized trials of radiotherapy in ductal carcinoma in situ of the breast. J Natl Cancer Inst Monogr. 2010;2010(41):162–177.
Van Zee KJ, White J, Morrow M, Harris JR. Ductal carcinoma in situ and microinvasive carcinoma. In: Harris JR, Lippman ME, Morrow M, Osborne CK (eds). Diseases of the breast. Philadelphia: Wolters Kluwer Health Adis; 2014.
Wapnir IL, Dignam JJ, Fisher B, et al. Long-term outcomes of invasive ipsilateral breast tumor recurrences after lumpectomy in NSABP B-17 and B-24 randomized clinical trials for DCIS. J Natl Cancer Inst. 2011;103(6):478–488.
Donker M, Litiere S, Werutsky G, et al. Breast-conserving treatment with or without radiotherapy in ductal carcinoma in situ: 15-year recurrence rates and outcome after a recurrence, from the EORTC 10853 randomized phase III trial. J Clin Oncol. 2013;31(32):4054–4059.
Cuzick J, Sestak I, Pinder SE, et al. Effect of tamoxifen and radiotherapy in women with locally excised ductal carcinoma in situ: long-term results from the UK/ANZ DCIS trial. Lancet Oncol. 2011;12(1):21–29.
Stuart KE, Houssami N, Taylor R, Hayen A, Boyages J. Long-term outcomes of ductal carcinoma in situ of the breast: a systematic review, meta-analysis and meta-regression analysis. BMC Cancer. 2015;15:890.
Cronin PA, Olcese C, Patil S, Morrow M, Van Zee KJ. Impact of age on risk of recurrence of ductal carcinoma in situ: outcomes of 2996 women treated with breast-conserving surgery over 30 years. Ann Surg Oncol. 2016;23(9):2816–2824.
Marinovich ML, Azizi L, Macaskill P, et al. The association of surgical margins and local recurrence in women with ductal carcinoma in situ treated with breast-conserving therapy: a meta-analysis. Ann Surg Oncol. 2016;23(12):3811–3821.
Klein J, Kong I, Paszat L, et al. Close or positive resection margins are not associated with an increased risk of chest wall recurrence in women with DCIS treated by mastectomy: a population-based analysis. Springerplus. 2015;4:335.
Carlson GW, Page A, Johnson E, Nicholson K, Styblo TM, Wood WC. Local recurrence of ductal carcinoma in situ after skin-sparing mastectomy. J Am Coll Surg. 2007;204(5):1074–1078 (discussion 1078-1080).
Owen D, Tyldesley S, Alexander C, et al. Outcomes in patients treated with mastectomy for ductal carcinoma in situ. Int J Radiat Oncol Biol Phys. 2013;85(3):e129–134.
Childs SK, Chen YH, Duggan MM, et al. Impact of margin status on local recurrence after mastectomy for ductal carcinoma in situ. Int J Radiat Oncol Biol Phys. 2013;85(4):948–952.
Fitzsullivan E, Lari SA, Smith B, et al. Incidence and consequence of close margins in patients with ductal carcinoma-in situ treated with mastectomy: is further therapy warranted? Ann Surg Oncol. 2013;20(13):4103–4112.
Chadha M, Portenoy J, Boolbol SK, Gillego A, Harrison LB. Is there a role for postmastectomy radiation therapy in ductal carcinoma in situ? Int J Surg Oncol. 2012;2012:423520.
Rashtian A, Iganej S, Amy Liu IL, Natarajan S. Close or positive margins after mastectomy for DCIS: pattern of relapse and potential indications for radiotherapy. Int J Radiat Oncol Biol Phys. 2008;72(4):1016–1020.
Rutter CE, Park HS, Killelea BK, Evans SB. Growing use of mastectomy for ductal carcinoma-in situ of the breast among young women in the United States. Ann Surg Oncol. 2015;22(7):2378–2386.
Park HL, Chang J, Lal G, Lal K, Ziogas A, Anton-Culver H. Trends in treatment patterns and clinical outcomes in young women diagnosed with ductal carcinoma in situ. Clin Breast Cancer. 2018;18(2):e179–e185.
Katz SJ, Lantz PM, Janz NK, et al. Patterns and correlates of local therapy for women with ductal carcinoma-in-situ. J Clin Oncol. 2005;23(13):3001–3007.
Parikh RR, Haffty BG, Lannin D, Moran MS. Ductal carcinoma in situ with microinvasion: prognostic implications, long-term outcomes, and role of axillary evaluation. Int J Radiat Oncol Biol Phys. 2012;82(1):7–13.
Sopik V, Sun P, Narod SA. Impact of microinvasion on breast cancer mortality in women with ductal carcinoma in situ. Breast Cancer Res Treat. 2018;167(3):787–795.
Sue GR, Lannin DR, Killelea B, Chagpar AB. Predictors of microinvasion and its prognostic role in ductal carcinoma in situ. Am J Surg. 2013;206(4):478–481.
Funding
The preparation of this study was funded in part by NIH/NCI Cancer Center Support Grant No. P30 CA008748.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Monica Morrow and Tari A. King have received honoraria from Genomic Health and Roche. Kimberly J. Van Zee served on the advisory board of Genomic Health in 2012. Anita Mamtani, Faina Nakhlis, Stephanie Downs-Canner, and Emily C. Zabor have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mamtani, A., Nakhlis, F., Downs-Canner, S. et al. Impact of Age on Locoregional and Distant Recurrence After Mastectomy for Ductal Carcinoma In Situ With or Without Microinvasion. Ann Surg Oncol 26, 4264–4271 (2019). https://doi.org/10.1245/s10434-019-07693-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07693-1