Abstract
Background
Ductal carcinoma in situ (DCIS) with microinvasion (DCISM) can be challenging in balancing the risks of overtreatment versus undertreatment. We compared DCISM, pure DCIS, and small volume (T1a) invasive ductal carcinoma (IDC) as related to histopathology, treatment patterns, and survival outcomes.
Methods
Women ages 18–90 years who underwent breast surgery for DCIS, DCISM, or T1a IDC were selected from the SEER Database (2004–2015). Multivariate logistic regression and Cox proportional hazards models were used to estimate the association of diagnosis with treatment and survival, respectively.
Results
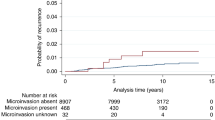
A total of 134,569 women were identified: 3.2% DCISM, 70.9% DCIS, and 25.9% with T1a IDC. Compared with invasive disease, DCISM was less likely to be ER+ or PR+ and more likely to be HER2+. After adjustment, DCIS and invasive patients were less likely to undergo mastectomy than DCISM patients (DCIS: OR 0.53, 95% CI 0.49–0.56; invasive: OR 0.86, CI 0.81–0.92). For those undergoing lumpectomy, the likelihood of receiving radiation was similar for DCISM and invasive patients but lower for DCIS patients (OR 0.57, CI 0.52–0.63). After adjustment, breast-cancer-specific survival was significantly different between DCISM and the other two groups (DCIS: HR 0.59, CI 0.43–0.8; invasive: HR 1.43, CI 1.04–1.96). However, overall survival was not significantly different between DCISM and invasive disease, whereas patients with DCIS had improved OS (HR 0.83, CI 0.75–0.93).
Conclusions
Although DCISM is a distinct entity, current treatment patterns and prognosis are comparable to those with small volume IDC. These findings may help providers counsel patients and determine appropriate treatment plans.

Similar content being viewed by others
References
Gradishar WJ, Anderson BO, Aft R, et al. NCCN guidelines: breast cancer, version 1. 2018. 20 March 2018.
Shapiro-Wright HM, Julian TB. Sentinel lymph node biopsy and management of the axilla in ductal carcinoma in situ. J Natl Cancer Inst Monogr. 2010;2010(41):145–149.
Hwang ES, Hyslop T, Lynch T, et al. The COMET (Comparison of Operative to Monitoring and Endocrine Therapy) Trial: a phase III randomized trial for low-risk ductal carcinoma in situ (DCIS). BMJ. 2018;9:e026797.
Elshof LE, Tryfonidis K, Slaets L, et al. Feasibility of a prospective, randomised, open-label, international multicentre, phase III, non-inferiority trial to assess the safety of active surveillance for low risk ductal carcinoma in situ - The LORD study. Eur J Cancer. 2015;51(12):1497–510.
Francis A, Fallowfield L, Rea D. The LORIS Trial: Addressing overtreatment of ductal carcinoma in situ. Clin oncol (R Coll Radiol (Great Britain)). 2015;27(1):6–8.
Parikh RR, Haffty BG, Lannin D, Moran MS. Ductal carcinoma in situ with microinvasion: prognostic implications, long-term outcomes, and role of axillary evaluation. Int J Radiat Oncol Biol Phys. 2012;82(1):7–13.
Li Y, Zhang S, Wei X, Zhang J. The clinical features and management of women with ductal carcinoma in situ with microinvasion: a retrospective cohort study. Int J Surg (London, Engl). 2015;19:91–4.
Fang Y, Wu J, Wang W, et al. Biologic behavior and long-term outcomes of breast ductal carcinoma in situ with microinvasion. Oncotarget. 2016;7(39):64182–90.
Wang W, Zhu W, Du F, Luo Y, Xu B. The demographic features, clinicopathological characteristics and cancer-specific outcomes for patients with microinvasive breast cancer: a SEER database analysis. Sci. Rep. 2017;7:42045.
Sopik V, Sun P, Narod SA. Impact of microinvasion on breast cancer mortality in women with ductal carcinoma in situ. Breast Cancer Res Treat. 2018;167(3):787–95.
Adjusted AJCC 6th ed. T, N, M, and Stage. National Cancer Institute’s Surveillance, Epidemiology, and End Results Program. https://seer.cancer.gov/seerstat/variables/seer/ajcc-stage/6th/#cs. Accessed 16 Apr 2019.
Hortobagyi GN, Connolly JL, D'Orsi CJ, et al. Breast. In: Amin MB, Gress DM, Meyer Vega LR, Edge SB, Greene FL, Byrd DR, Brookland RK, Washington MK, Compton CC, editors. AJCC cancer staging manual. 8th edn. New York, NY: Springer; 2016.
Wan ZB, Gao HY, Wei L, et al. Expression of estrogen receptor, progesterone receptor, human epidermal growth factor receptor 2, and Ki-67 in ductal carcinoma in situ (DCIS) and DCIS with microinvasion. Medicine (Baltimore). 2018;97(44):e13055.
Grimm LJ, Ryser MD, Partridge AH, et al. Surgical upstaging rates for vacuum assisted biopsy proven DCIS: implications for active surveillance trials. Ann Surg Oncol. 2017;24(12):3534–3540.
de Paz Villanueva CC, Bonev V, Senthil M, et al. Factors associated with underestimation of invasive cancer in patients with ductal carcinoma in situ: precautions for active surveillance. JAMA Surg. 2017;152(11):1007–14.
Kurniawan ED, Rose A, Mou A, et al. Risk factors for invasive breast cancer when core needle biopsy shows ductal carcinoma in situ. Arch Surg. 2010;145(11):1098–104.
Chin-Lenn L, Mack LA, Temple W, et al. Predictors of treatment with mastectomy, use of sentinel lymph node biopsy and upstaging to invasive cancer in patients diagnosed with breast ductal carcinoma in situ (DCIS) on core biopsy. Ann Surg Oncol. 2014;21(1):66–73.
Burstein HJ, Polyak K, Wong JS, Lester SC, Kaelin CM. Ductal carcinoma in situ of the breast. N Engl J Med. 2004;350(14):1430–41.
Narod SA, Sopik V. Is invasion a necessary step for metastases in breast cancer? Breast Cancer Res Treat. 2018;169(1):9–23.
Giannakeas V, Sopik V, Narod SA. A comparison of two models for breast cancer mortality for women with ductal carcinoma in situ: an SEER-based analysis. Breast Cancer Res Treat. 2018;169(3):587–94.
Hwang ES, DeVries S, Chew KL, et al. Patterns of chromosomal alterations in breast ductal carcinoma in situ. Clin Cancer Res. 2004;10(15):5160–7.
Abba MC, Gong T, Lu Y, et al. A molecular portrait of high-grade ductal carcinoma in situ. Cancer Res. 2015;75(18):3980–90.
Ellsworth RE, Vertrees A, Love B, Hooke JA, Ellsworth DL, Shriver CD. Chromosomal alterations associated with the transition from in situ to invasive breast cancer. Ann Surg Oncol. 2008;15(9):2519–25.
Iakovlev VV, Arneson NC, Wong V, et al. Genomic differences between pure ductal carcinoma in situ of the breast and that associated with invasive disease: a calibrated aCGH study. Clin Cancer Res. 2008;14(14):4446–54.
Acknowledgment
The Surveillance, Epidemiology, and End Results (SEER) database is supported by the Surveillance Research Program in the National Cancer Institute’s Division of Cancer Control and Population Sciences. The SEER database is the source of the de-identified data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors. Dr. R. Greenup is supported by the National Institutes of Health Office of Women’s Research Building Interdisciplinary Research Careers in Women’s Health K12HD043446 (PI: Andrews). Dr. O. Fayanju is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH) under Award Number Award Number 1KL2TR002554 (PI: Svetkey). This work is also supported by the Duke Cancer Institute through NIH grant P30CA014236 (PI: Kastan). The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Champion, C.D., Ren, Y., Thomas, S.M. et al. DCIS with Microinvasion: Is It In Situ or Invasive Disease?. Ann Surg Oncol 26, 3124–3132 (2019). https://doi.org/10.1245/s10434-019-07556-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07556-9