Abstract
Background
Increasing the interval from completion of neoadjuvant therapy to surgery beyond 8 weeks is associated with increased response of rectal cancer to neoadjuvant therapy. However, reports are conflicting on whether extending the time to surgery is associated with increased perioperative morbidity.
Methods
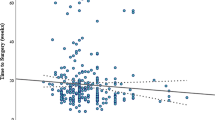
Patients who presented with a tumor within 15 cm of the anal verge in 2009–2015 were grouped according to the interval between completion of neoadjuvant therapy and surgery: < 8 weeks, 8–12 weeks, and 12–16 weeks.
Results
Among 607 patients, the surgery was performed at < 8 weeks in 317 patients, 8–12 weeks in 229 patients, and 12–16 weeks in 61 patients. Patients who underwent surgery at 8–12 weeks and patients who underwent surgery at < 8 weeks had comparable rates of complications (37% and 44%, respectively). Univariable analysis identified male sex, earlier date of diagnosis, tumor location within 5 cm of the anal verge, open operative approach, abdominoperineal resection, and use of neoadjuvant chemoradiotherapy alone to be associated with higher rates of complications. In multivariable analysis, male sex, tumor location within 5 cm of the anal verge, open operative approach, and neoadjuvant chemoradiotherapy administered alone were independently associated with the presence of a complication. The interval between neoadjuvant therapy and surgery was not an independent predictor of postoperative complications.
Conclusions
Delaying surgery beyond 8 weeks from completion of neoadjuvant therapy does not appear to increase surgical morbidity in rectal cancer patients.
Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30.
Rodel C, Graeven U, Fietkau R, et al. Oxaliplatin added to fluorouracil-based preoperative chemoradiotherapy and postoperative chemotherapy of locally advanced rectal cancer (the German CAO/ARO/AIO-04 study): final results of the multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2015;16:979–89.
Cunningham D, Atkin W, Lenz HJ, et al. Colorectal cancer. Lancet. 2010;375:1030–47.
Ding P, Liska D, Tang P, et al. Pulmonary recurrence predominates after combined modality therapy for rectal cancer: an original retrospective study. Ann Surg. 2012;256:111–6.
Tulchinsky H, Shmueli E, Figer A, Klausner JM, Rabau M. An interval > 7 weeks between neoadjuvant therapy and surgery improves pathologic complete response and disease-free survival in patients with locally advanced rectal cancer. Ann Surg Oncol. 2008;15:2661–7.
Habr-Gama A, Perez RO, Proscurshim I, et al. Interval between surgery and neoadjuvant chemoradiation therapy for distal rectal cancer: does delayed surgery have an impact on outcome? Int J Radiat Oncol Biol Phys. 2008;71:1181–8.
Sloothaak DA, Geijsen DE, van Leersum NJ, et al. Optimal time interval between neoadjuvant chemoradiotherapy and surgery for rectal cancer. Br J Surg. 2013;100:933–9.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Francois Y, Nemoz CJ, Baulieux J, et al. Influence of the interval between preoperative radiation therapy and surgery on downstaging and on the rate of sphincter-sparing surgery for rectal cancer: the Lyon R90-01 randomized trial. J Clin Oncol. 1999;17:2396.
Kalady MF, de Campos-Lobato LF, Stocchi L, et al. Predictive factors of pathologic complete response after neoadjuvant chemoradiation for rectal cancer. Ann Surg. 2009;250:582–9.
Huntington CR, Boselli D, Symanowski J, Hill JS, Crimaldi A, Salo JC. Optimal timing of surgical resection after radiation in locally advanced rectal adenocarcinoma: an analysis of the national cancer database. Ann Surg Oncol. 2016;23:877–87.
Sun Z, Adam MA, Kim J, Shenoi M, Migaly J, Mantyh CR. Optimal timing to surgery after neoadjuvant chemoradiotherapy for locally advanced rectal cancer. J Am Coll Surg. 2016;222:367–74.
Lefevre JH, Mineur L, Kotti S, et al. Effect of interval (7 or 11 weeks) Between neoadjuvant radiochemotherapy and surgery on complete pathologic response in rectal cancer: a multicenter, randomized, controlled trial (GRECCAR-6). J Clin Oncol. 2016;34:3773–80.
Garcia-Aguilar J, Chow OS, Smith DD, et al. Effect of adding mFOLFOX6 after neoadjuvant chemoradiation in locally advanced rectal cancer: a multicentre, phase 2 trial. Lancet Oncol. 2015;16:957–66.
Cercek A, Roxburgh CSD, Strombom P, et al. Adoption of total neoadjuvant therapy for locally advanced rectal cancer. JAMA Oncol. 2018;4:e180071
Smith JJ, Garcia-Aguilar J. Advances and challenges in treatment of locally advanced rectal cancer. J Clin Oncol. 2015;33:1797–808.
Washington MK, Berlin J, Branton P, et al. Protocol for the examination of specimens from patients with primary carcinoma of the colon and rectum. Arch Pathol Lab Med. 2009;133:1539–51.
Strong VE, Selby LV, Sovel M, et al. Development and assessment of Memorial Sloan Kettering Cancer Center’s Surgical Secondary Events grading system. Ann Surg Oncol. 2015;22:1061–7.
Wiatrek RL, Thomas JS, Papaconstantinou HT. Perineal wound complications after abdominoperineal resection. Clin Colon Rectal Surg. 2008;21:76–85.
Acknowledgment
This research was supported in part by the NCI Grant P30 CA008748. The authors gratefully acknowledge Arthur Gelmis for editing the manuscript.
Funding
NCI P30 CA008748.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Roxburgh, C.S.D., Strombom, P., Lynn, P. et al. Role of the Interval from Completion of Neoadjuvant Therapy to Surgery in Postoperative Morbidity in Patients with Locally Advanced Rectal Cancer. Ann Surg Oncol 26, 2019–2027 (2019). https://doi.org/10.1245/s10434-019-07340-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07340-9