Abstract
Background
Patients undergoing oncologic surgery are at risk for persistent postoperative opioid use. As a quality improvement initiative, this study sought to characterize provider perceptions regarding opioid-prescribing after oncologic procedures.
Methods
Surgical oncology attending physicians, clinical fellows, and advanced practice providers (APPs) at a high-volume cancer center were surveyed before and after educational sessions focusing on the opioid epidemic with review of departmental data.
Results
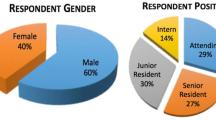
The pre-education response rates were 72 (70%) of 103: 22 (65%) of 34 attending physicians, 19 (90%) of 21 fellows, and 31 (65%) of 48 APPs. For five index operations (open abdominal resection, laparoscopic colectomy, wide local excision, thyroidectomy, port), the fellows answered that patients should stop receiving opioids sooner than recommended by the attending surgeons or APPs. For four of five procedures, the APPs recommended higher discharge opioid prescriptions than the attending surgeons or fellows. Almost half of the providers (n = 46, 45%) responded to both the pre- and post-education surveys. After the intervention, the providers recommended lower numbers of opioid pills and indicated that patients should be weaned from opioids sooner for all the procedures. Compared with pre-education, more providers agreed post-education that discharge opioid prescriptions should be based on a patient’s last 24 h of inpatient opioid use (83 vs 91%; p = 0.006). The providers who did not attend a session showed no difference in perceptions or recommendations at the repeat assessment.
Conclusions
Variation exists in perioperative opioid-prescribing among provider types, with those most involved in daily care and discharge processes generally recommending more opioids. After education, providers lowered discharge opioid recommendations and thought patients should stop receiving opioids sooner. The next steps include assessing for quantitative changes in opioid-prescribing and implementing standardized opioid prescription algorithms.


Similar content being viewed by others
References
Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths–United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2016;64:1378–82.
Kenan K, Mack K, Paulozzi L. Trends in prescriptions for oxycodone and other commonly used opioids in the United States, 2000–2010. Open Med. 2012;6:e41–7.
Hah JM, Bateman BT, Ratliff J, Curtin C, Sun E. Chronic opioid use after surgery: implications for perioperative management in the face of the opioid epidemic. Anesth Analg. 2017;125:1733–40.
Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152:e170504.
Lee JS-J, Hu HM, Edelman AL, et al. New persistent opioid use among patients with cancer after curative-intent surgery. J Clin Oncol. 2017;35:4042–9.
Tuminello S, Schwartz R, Liu B, et al. Opioid use after open resection or video-assisted thoracoscopic surgery for early-stage lung cancer. JAMA Oncol. 2018;4:1611–3.
Alvarez MP, Foley KE, Zebley DM, Fassler SA. Comprehensive enhanced recovery pathway significantly reduces postoperative length of stay and opioid usage in elective laparoscopic colectomy. Surg Endosc. 2015;29:2506–11.
King AB, Spann MD, Jablonski P, Wanderer JP, Sandberg WS, McEvoy MD. An enhanced recovery program for bariatric surgical patients significantly reduces perioperative opioid consumption and postoperative nausea. Surg Obes Relat Dis. 2018;14:849–56. https://doi.org/10.1016/j.soard.2018.02.010.
Grant MC, Sommer PM, He C, et al. Preserved analgesia with reduction in opioids through the use of an acute pain protocol in enhanced recovery after surgery for open hepatectomy. Regional Anesth Pain Med. 2017;42:451–7.
Brandal D, Keller MS, Lee C, et al. Impact of enhanced recovery after surgery and opioid-free anesthesia on opioid prescriptions at discharge from the hospital: a historical-prospective study. Anesth Analg. 2017;125:1784–92.
Thiels CA, Anderson SS, Ubl DS, et al. Wide variation and overprescription of opioids after elective surgery. Ann Surg. 2017;266:564–73.
Hill MV, McMahon ML, Stucke RS, Barth RJ Jr. Wide variation and excessive dosage of opioid prescriptions for common general surgical procedures. Ann Surg. 2017;265:709–14.
Eid AI, DePesa C, Nordestgaard AT, et al. Variation of opioid-prescribing patterns among patients undergoing similar surgery on the same acute care surgery service of the same institution: time for standardization? Surgery. 2018;164:926–30.
Overton HN, Hanna MN, Bruhn WE, Hutfless S, Bicket MC, Makary MA. Opioid-prescribing guidelines for common surgical procedures: an expert panel consensus. J Am Coll Surg. 2018;227:411–8.
Thiels CA, Ubl DS, Yost KJ, et al. Results of a prospective, multicenter initiative aimed at developing opioid-prescribing guidelines after surgery. Ann Surg. 2018;268:457–68.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Informat. 2009;42:377–81.
Newhook TE, Vreeland TJ, Dewhurst WL, et al. Clinical factors associated with practice variation in discharge opioid prescriptions after pancreatectomy. Ann Surg. 2018. https://doi.org/10.1097/SLA.0000000000003112.
Lev R, Lee O, Petro S, et al. Who is prescribing controlled medications to patients who die of prescription drug abuse? Am J Emerg Med. 2016;34:30–5.
Funding
Dr. Heather Lillemoe is supported by National Institutes of Health Grant T32CA009599 and the MD Anderson Cancer Center support Grant P30 CA016672.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lillemoe, H.A., Newhook, T.E., Vreeland, T.J. et al. Educating Surgical Oncology Providers on Perioperative Opioid Use: Results of a Departmental Survey on Perceptions of Opioid Needs and Prescribing Habits. Ann Surg Oncol 26, 2011–2018 (2019). https://doi.org/10.1245/s10434-019-07321-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07321-y