Abstract
Background
A positive lumpectomy margin after breast-conserving surgery (BCS) is a significant predictor for ipsilateral cancer recurrence. The MarginProbe, a Food and Drug Administration (FDA)-approved device for intraoperative assessment of lumpectomy margins, is associated with a reduction in re-excision surgery. This study aimed to evaluate the relationship of mammographic breast density (MBD) and clinicopathologic characteristics with margin status in women undergoing BCS with the MarginProbe.
Methods
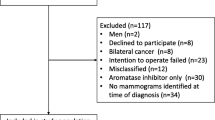
The institutional database was queried for patients with breast cancer who had BCS with the MarginProbe from 2013 to 2017. Clinicopathologic characteristics were collected. The study defined MBD as less dense (Breast Imaging Reporting and Data System [BI-RADS] A and B) and more dense (BI-RADS C and D). A positive margin was defined as smaller than 1 mm. Pearson Chi square and uni- and multivariate logistic regression were performed.
Results
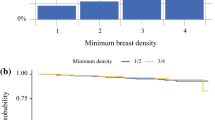
Of 1734 patients, 341 met the study criteria. The median patient age was 63 years. The patients with higher mammographic density were younger (p < 0.0001) and had a lower body mass index (BMI) (p < 0.0001). The patients with higher MBD were more likely to present with a palpable mass (p = 0.0360). Of the 341 patients, 135 (39.6%) had one or more positive margins on the main specimen, and 101 (74.8%) were converted to final negative margins after the MarginProbe directed re-excisions. Positive final margins were associated with larger tumor size (p = 0.0242) and more advanced stage of disease at diagnosis (p = 0.0255).
Conclusions
In this study of patients undergoing BCS, breast density was not correlated with the likelihood of a positive margin. The presence of positive final lumpectomy margins was associated with older age and more extensive disease.
Similar content being viewed by others
References
Schnabel F, Boolbol SK, Gittleman M, Karni T, Tafra L, Feldman S et al. A randomized prospective study of lumpectomy margin assessment with use of MarginProbe in patients with nonpalpable breast malignancies. Ann Surg Oncol. 2014:21:1589–95.
A. C. Society. Breast cancer facts and figures 2017–2018. Atlanta: A.C. Society; 2017. p 1–44.
Thill M, Dittmer C, Baumann K, Friedrichs K, Blohmer JU. MarginProbe(R): final results of the German post-market study in breast-conserving surgery of ductal carcinoma in situ. Breast. 2014;23:94–6.
Zysk AM, Chen K, Gabrielson E, Tafra L, May Gonzalez EA, Canner JK et al. Intraoperative assessment of final margins with a handheld optical imaging probe during breast-conserving surgery may reduce the reoperation rate: results of a multicenter study. Ann Surg Oncol. 2015;22:3356–62.
Edwards BL, Guidry CA, Larson KN, Novicoff WM, Harvey JA, Schroen AT. Does mammographic density have an impact on the margin re-excision rate after breast-conserving surgery? Ann Surg Oncol. 2016;23:782–8.
Blohmer JU, Tanko J, Kueper J, Groß J, Völker R, Machleidt A. MarginProbe(c) reduces the rate of re-excision following breast-conserving surgery for breast cancer. Arch Gynecol Obstet. 2016;294:361–7.
Rivera RJ, Holmes DR, Tafra L. Analysis of the impact of intraoperative margin assessment with adjunctive use of MarginProbe versus standard of care on tissue volume removed. Int J Surg Oncol. 2012;2012:868623.
Allweis TM, Kaufman Z, Lelcuk S, Pappo I, Karni T, Schneebaum S et al. A prospective, randomized, controlled, multicenter study of a real-time, intraoperative probe for positive margin detection in breast-conserving surgery. Am J Surg. 2008;196:483–9.
Radiology ACo. ACR BI-RADS atlas. In: Mammography. 5th ed. 2013, pp. 121–140.
Morrow M, Van Zee KJ, Solin LJ, Houssami N, Chavez-MacGregor M, Harris JR et al. Society of Surgical Oncology–American Society for Radiation Oncology–American Society of Clinical Oncology Consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in ductal carcinoma in situ. Ann Surg Oncol. 2016;23:3801–10.
Schnabel FR, Allweis TA. Breast density and the risk for positive lumpectomy margins. J Clin Oncol. 2015;33(28 Suppl):50.
Police A, Lin E, Lane K. Intraoperative margin assessment with the MarginProbe at different mammographic breast densities. J Clin Oncol. 2015;33(28 Suppl):47.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None of the authors have any honoraria, consulting fees or funding from the company and have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gooch, J.C., Yoon, E., Chun, J. et al. The Relationship of Breast Density and Positive Lumpectomy Margins. Ann Surg Oncol 26, 1729–1736 (2019). https://doi.org/10.1245/s10434-019-07295-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07295-x