Abstract
Objective
The aim of this study was to evaluate socioeconomic discrepancies in current treatment approaches and survival trends among patients with intrahepatic cholangiocarcinoma (ICC).
Methods
The 2004–2015 National Cancer Database was retrospectively analyzed for histopathologically proven ICC. Treatment predictors were evaluated using multinomial logistic regression and overall survival via multivariable Cox models.
Results
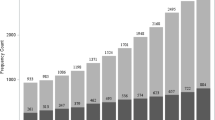
Overall, 12,837 ICC patients were included. Multiple factors influenced treatment allocation, including age, education, comorbidities, cancer stage, grade, treatment center, and US state region (multivariable p < 0.05). The highest surgery rates were observed in the Middle Atlantic (28.7%) and lowest rates were observed in the Mountain States (18.4%). Decreased ICC treatment likelihood was observed for male African Americans with Medicaid insurance and those with low income (multivariable p < 0.05). Socioeconomic treatment discrepancies translated into decreased overall survival for patients of male sex (vs. female; hazard ratio [HR] 1.21, 95% confidence interval [CI] 1.16–1.26, p < 0.001), with low income (< $37,999 vs. ≥ $63,000 annually; HR 1.07, 95% CI 1.01–1.14, p = 0.032), and with Medicaid insurance (vs. private insurance; HR 1.13, 95% CI 1.04–1.23, p = 0.006). Both surgical and non-surgical ICC management showed increased survival compared with no treatment, with the longest survival for surgery (5-year overall survival for surgery, 33.5%; interventional oncology, 11.8%; radiation oncology/chemotherapy, 4.4%; no treatment, 3.3%). Among non-surgically treated patients, interventional oncology yielded the longest survival versus radiation oncology/chemotherapy (HR 0.73, 95% CI 0.65–0.82, p < 0.001).
Conclusions
ICC treatment allocation and outcome demonstrated a marked variation depending on socioeconomic status, demography, cancer factors, and US geography. Healthcare providers should address these discrepancies by providing surgery and interventional oncology as first-line treatment to all eligible patients, with special attention to the vulnerable populations identified in this study.




Similar content being viewed by others
References
Patel T. Increasing incidence and mortality of primary intrahepatic cholangiocarcinoma in the United States. Hepatology. 2001;33(6):1353–57.
Shaib Y, El-Serag HB. The epidemiology of cholangiocarcinoma. Semin Liver Dis. 2004;24(2):115–25.
Vauthey JN, Blumgart LH. Recent advances in the management of cholangiocarcinomas. Semin Liver Dis. 1994;14(2):109–14.
DeOliveira ML, Cunningham SC, Cameron JL, et al. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg. 2007;245(5):755–62.
Khan SA, Taylor-Robinson SD, Toledano MB, Beck A, Elliott P, Thomas HC. Changing international trends in mortality rates for liver, biliary and pancreatic tumours. J Hepatol. 2002;37(6):806–13.
Yao KJ, Jabbour S, Parekh N, Lin Y, Moss RA. Increasing mortality in the United States from cholangiocarcinoma: an analysis of the National Center for Health Statistics Database. BMC Gastroenterol. 2016;16:117.
Esnaola NF, Meyer JE, Karachristos A, Maranki JL, Camp ER, Denlinger CS. Evaluation and management of intrahepatic and extrahepatic cholangiocarcinoma. Cancer. 2016;122(9):1349–69.
Khan SA, Davidson BR, Goldin R, et al. Guidelines for the diagnosis and treatment of cholangiocarcinoma: consensus document. Gut. 2002;51 Suppl 6:Vi1–9.
Jarnagin WR, Shoup M. Surgical management of cholangiocarcinoma. Semin Liver Dis. 2004;24(2):189–99.
Valle J, Wasan H, Palmer DH, et al. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 2010;362(14):1273–81.
Konstantinidis IT, Arkadopoulos N, Ferrone CR. Surgical management of intrahepatic cholangiocarcinoma in the modern era: advances and challenges. Chin Clin Oncol. 2016;5(1):9.
Dwyer-Lindgren L, Flaxman AD, Ng M, Hansen GM, Murray CJ, Mokdad AH. Drinking patterns in US counties from 2002 to 2012. Am J Public Health. 2015;105(6):1120–7.
Yoon Y-H, Chen CM. Surveillance report #105: Liver cirrhosis mortality in the United States: national, state, and regional trends, 2000–2013. Arlington, VA. Department of Health and Human Services, Public Health Service, National Institutes of Health; 2016.
Overweight and 0besity. 2018. https://www.cdc.gov/obesity/index.html.
Younossi ZM, Stepanova M, Afendy M, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol. 2011;9(6):524–30.e521; quiz e560.
Sarmiento JM, Nagorney DM. Hepatic resection in the treatment of perihilar cholangiocarcinoma. Surg Oncol Clin N Am. 2002;11(4):893–908, viii–ix.
Lewis CE, Smith E, Kercher C, Spitznagel E. Predictors of mortality in alcoholic men: a 20-year follow-up study. Alcohol Clin Exp Res. 1995;19(4):984–91.
Leyland AH, Dundas R, McLoone P, Boddy FA. Cause-specific inequalities in mortality in Scotland: two decades of change. A population-based study. BMC Public Health. 2007;7:172.
Najman JM, Williams GM, Room R. Increasing socioeconomic inequalities in male cirrhosis of the liver mortality: Australia 1981–2002. Drug Alcohol Rev. 2007;26(3):273–8.
Jepsen P, Vilstrup H, Andersen PK, Sorensen HT. Socioeconomic status and survival of cirrhosis patients: a Danish nationwide cohort study. BMC Gastroenterol. 2009;9:35.
Pinter M, Trauner M, Peck-Radosavljevic M, Sieghart W. Cancer and liver cirrhosis: implications on prognosis and management. ESMO Open. 2016;1(2):e000042.
Arpey NC, Gaglioti AH, Rosenbaum ME. How socioeconomic status affects patient perceptions of health care: a qualitative study. J Prim Care Commun Health. 2017;8(3):169–75.
Kullgren JT, Galbraith AA, Hinrichsen VL, et al. Health care use and decision-making among lower-income families in high-deductible health plans. Arch Intern Med. 2010;170(21):1918–25.
Hibbard JH, Cunningham PJ. How engaged are consumers in their health and health care, and why does it matter? Res Brief. 2008;8:1–9.
Trivedi AN, Rakowski W, Ayanian JZ. Effect of cost sharing on screening mammography in Medicare health plans. N Engl J Med. 2008;358(4):375–83.
Trivedi AN, Moloo H, Mor V. Increased ambulatory care copayments and hospitalizations among the elderly. N Engl J Med. 2010;362(4):320–8.
Nakeeb A, Tran KQ, Black MJ, et al. Improved survival in resected biliary malignancies. Surgery. 2002;132(4):555–63; discission 563–554.
Bridgewater J, Galle PR, Khan SA, et al. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol. 2014;60(6):1268–89.
Shindoh J. Ablative therapies for intrahepatic cholangiocarcinoma. Hepatobil Surg Nutr. 2017;6(1):2–6.
Zhang SJ, Hu P, Wang N, et al. Thermal ablation versus repeated hepatic resection for recurrent intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2013;20(11):3596–602.
Author information
Authors and Affiliations
Contributions
Conceptualization: JU, HSK. Methodology: JU. Validation: JU, HSK. Formal analysis: JU. Investigation: JU, CMS, HSK. Resources: CC, JL, SMS, HSK. Data curation: JU, CMS, HSK. Writing of the original draft: JU, CMS, CC, SAK, JL, SMS, HSK. Visualization: JU. Supervision: HSK. Project administration: CC, SAK, JL, SMS, HSK.
Corresponding author
Ethics declarations
DISCLOSURE
Johannes Uhlig, Cortlandt M. Sellers, Charles Cha, Sajid A. Khan, Jill Lacy, Stacey M. Stein, and Hyun S. Kim have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Uhlig, J., Sellers, C.M., Cha, C. et al. Intrahepatic Cholangiocarcinoma: Socioeconomic Discrepancies, Contemporary Treatment Approaches and Survival Trends from the National Cancer Database. Ann Surg Oncol 26, 1993–2000 (2019). https://doi.org/10.1245/s10434-019-07175-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07175-4