Abstract
Background
Diagnostic hemithyroidectomy (HT) is the most widely recommended surgical procedure for a nodule with indeterminate cytology; however, additional details may make initial total thyroidectomy (TT) preferable. We sought to identify patient-specific factors (PSFs) associated with initial TT in patients with indeterminate thyroid nodules.
Methods
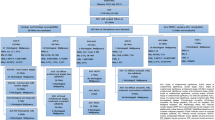
Retrospective analysis of all patients with a thyroid nodule ≥ 1 cm and initial cytology of atypia of undetermined significance or suspicious for follicular neoplasm between 2012 and 2015 who underwent thyroidectomy. Medical records were reviewed for patient demographics, neck symptoms, nodule size, cytology, molecular test results, final histopathology, and additional PSFs influencing surgical management. Variables were analyzed to determine associations with the use of initial TT. Logistic regression analyses were performed to identify independent associations.
Results
Of 325 included patients, 182/325 (56.0%) had HT and 143/325 (44.0%) had TT. While patient age and sex, nodule size, and cytology result were not associated with initial treatment, five PSFs were associated with initial TT (p < 0.0001). These included contralateral nodules, hypothyroidism, fluorodeoxyglucose avidity on positron emission tomography scan, family history of thyroid cancer, and increased surgical risk. At least one PSF was present in 126/143 (88.1%) TT patients versus 47/182 (25.8%) HT patients (p < 0.0001). Multivariate logistic regression analysis demonstrated that these variables were the strongest independent predictor of TT (odds ratio 45.93, 95% confidence interval 18.80–112.23, p < 0.001).
Conclusions
When surgical management of an indeterminate cytology thyroid nodule was performed, several PSFs were associated with a preference by surgeons and patients for initial TT, which may be useful to consider in making decisions on initial operative extent.
Similar content being viewed by others
References
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29.
Popoveniuc G, Jonklaas J. Thyroid nodules. Med Clin North Am. 2012;96:329–49.
Yassa L, Cibas ES, Benson CB, et al. Long-term assessment of a multidisciplinary approach to thyroid nodule diagnostic evaluation. Cancer 2007;111:508–16.
Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26:1–133.
Gharib H, Papini E, Paschke R, Buick DS, Valcavi R, Hegedus L, et al. AACE/AME/ETA Task Force on Thyroid Nodules. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules: executive summary of recommendations. J Endocrinol Invest. 2010;33:51–56.
Bongiovanni M, Spitale A, Faquin WC, Mazzucchelli L, Baloch ZW. The Bethesda System for Reporting Thyroid Cytopathology: a meta-analysis. Acta Cytol. 2012;56:333–9.
Baloch ZW, Livolsi VA. Follicular-patterned lesions of the thyroid: the bane of the pathologist. Am J Clin Pathol. 2002;117:143–50.
Nayar R, Ivanovic M. The indeterminate thyroid fine-needle aspiration: experience from an academic center using terminology similar to that proposed in the 2007 National Cancer Institute Thyroid Fine Needle Aspiration State of the Science Conference. Cancer. 2009;117:195–202.
Cibas ES, Ali SZ. The Bethesda system for reporting thyroid cytopathology. Thyroid. 2009;19:1159–65.
Alexander EK, Kennedy GC, Baloch ZW, et al. Preoperative diagnosis of benign thyroid nodules with indeterminate cytology. N Engl J Med. 2012;367:705–15.
Adam MA, Thomas S, Youngwirth L, Hyslop T, Reed SD, Scheri RP, et al. Is there a minimum number of thyroidectomies a surgeon should perform to optimize patient outcomes? Ann Surg. 2017;265:402–7.
Nikiforov YE, Seethala RR, Tallini G, et al. Nomenclature revision for encapsulated follicular variant of papillary thyroid carcinoma: a paradigm shift to reduce overtreatment of indolent tumors. JAMA Oncol. 2016;2:1023–9.
Shapiro S, Pharaon M, Kellermeyer B. Cost-effectiveness of gene expression classifier testing of indeterminate thyroid nodules utilizing a real cohort comparator. Otolaryngol Head Neck Surg. 2017;157:596–601.
Hang JF, Westra WH, Cooper DS, Ali SZ. The impact of noninvasive follicular thyroid neoplasm with papillary-like nuclear features on the performance of the Afirma gene expression classifier. Cancer. 2017;125:683–91.
Yip L, Sosa JA. Molecular-directed treatment of differentiated thyroid cancer: advances in diagnosis and treatment. JAMA Surg. 2016;151:663–70.
Yip L, Wharry LI, Armstrong MJ, et al. A clinical algorithm for fine-needle aspiration molecular testing effectively guides the appropriate extent of initial thyroidectomy. Ann Surg 2014;260:163–8.
Patel SG, Carty SE, McCoy KL, et al. Preoperative detection of RAS mutation may guide extent of thyroidectomy. Surgery. 2017;161:168–75.
Li H, Robinson KA, Anton B, Saldanha IJ, Ladenson PW. Cost-effectiveness of a novel molecular test for cytologically indeterminate thyroid nodules. J Clin Endocrinol Metab. 2011;96:E1719–26.
Duick DS, Klopper JP, Diggans JC, Friedman L, Kennedy GC, Lanman RB, McIver B. The impact of benign gene expression classifier test results on the endocrinologist-patient decision to operate on patients with thyroid nodules with indeterminate fine-needle aspiration cytopathology. Thyroid. 2012;22:996–1001.
Lee L, How J, Tabah RJ, Mitmaker EJ. Cost-effectiveness of molecular testing for thyroid nodules with atypia of undetermined significance cytology. J Clin Endocrinol Metab. 2014;99:2674–82.
Labourier E. Utility and cost-effectiveness of molecular testing in thyroid nodules with indeterminate cytology. Clin Endocrinol (Oxf) 2016;85:624–31.
Wu JX, Lam R, Levin M, Rao J, Sullivan PS, Yeh MW. Effect of malignancy rates on cost-effectiveness of routine gene expression classifier testing for indeterminate thyroid nodules. Surgery. 2016;159:118–26.
Strickland KC, Howitt BE, Marqusee E, Alexander EK, Cibas ES, Krane JF, Barletta JA. The impact of non-invasive follicular variant of papillary thyroid carcinoma on rates of malignancy for fine-needle aspiration diagnostic categories. Thyroid. 2015;25:987–92.
Howitt BE, Chang S, Eszlinger M, Paschke R, Drage MG, Krane JF, Barletta JA. Fine-needle aspiration diagnoses of noninvasive follicular variant of papillary thyroid carcinoma. Am J Clin Pathol. 2015;144:850–7.
Maletta F, Massa F, Torregrossa L, et al. Cytological features of “noninvasive follicular thyroid neoplasm with papillary-like nuclear features” and their correlation with tumor histology. Hum Pathol. 2016;54:134–42.
Acknowledgements
None.
Disclosures
Trevor E. Angell has received research support from Veracyte Inc., and Erik K. Alexander is a consultant for Veracyte, Inc. Chirag M. Vyas, Justine A. Barletta, Edmund S. Cibas, Nancy L. Cho, Gerard M. Doherty, Atul A. Gawande, Brooke E. Howitt, Jeffrey F. Krane, Ellen Marqusee, Kyle C. Strickland, Francis D. Moore Jr, and Matthew Nehs have no relevant conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Angell, T.E., Vyas, C.M., Barletta, J.A. et al. Reasons Associated with Total Thyroidectomy as Initial Surgical Management of an Indeterminate Thyroid Nodule. Ann Surg Oncol 25, 1410–1417 (2018). https://doi.org/10.1245/s10434-018-6421-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6421-x