Abstract
Background
A relationship between sarcopenia diagnosed by skeletal muscle area (SMA) and poor prognosis in cancer patients has recently been reported. This study aimed to clarify the clinical significance of postoperatively decreased SMA in patients with early non-small cell lung cancer (NSCLC).
Methods
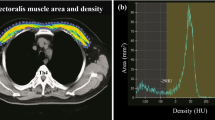
This study selected 101 patients with pathologic stage 1 NSCLC who had undergone pre- and postoperative (~ 1 year) computed tomography scans and lobectomy between 2005 and 2010 at Kyushu University Hospital. The post/pre ratio was defined as the postoperative normalized SMA (cm2/m2) at the 12th thoracic vertebra level divided by the preoperative normalized SMA. The cutoff value for the post/pre ratio was set at 0.9.
Results
The study classified 31 patients (30.7%) as having decreased SMA. Poor performance status (PS) was significantly associated with decreased SMA (p = 0.048). The patients with decreased SMA had a significantly shorter disease-free survival (DFS) (p < 0.001) and overall survival (OS) (p < 0.001) than the other patients. Decreased SMA was found to be an independent prognostic factor for DFS (p = 0.010) and OS (p = 0.0072). The independent risk factors for skeletal muscle loss included poor PS (PS ≥ 1) and obstructive ventilatory impairment [forced expiratory volume (FEV) 1% < 70%].
Conclusions
Skeletal muscle loss after surgery is significantly associated with postoperative poor outcomes for patients with early NSCLC. Patients with poor PS, obstructive ventilatory impairment, or both need careful support to maintain their skeletal muscle mass. Future prospective studies may clarify whether physical activity and nutritional support improve postoperative prognosis.


Similar content being viewed by others
References
Epidemiologic and methodologic problems in determining nutritional status of older persons. Proceedings of a conference at Albuquerque, New Mexico, 19–21 October 1988. Am J Clin Nutr. 1989;50(5 Suppl):1121–235.
Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr. 1997;127(5 Suppl):990s–91s.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–23.
Tanimoto Y, Watanabe M, Sun W, et al. Association between muscle mass and disability in performing instrumental activities of daily living (IADL) in community-dwelling elderly in Japan. Arch Gerontol Geriatrics. 2012;54:e230–3.
Bahat G, Tufan A, Tufan F, et al. Cutoff points to identify sarcopenia according to European Working Group on Sarcopenia in Older People (EWGSOP) definition. Clin Nutr Edinburgh Scotland. 2016;35:1557–63.
Sanada K, Miyachi M, Tanimoto M, et al. A cross-sectional study of sarcopenia in Japanese men and women: reference values and association with cardiovascular risk factors. Eur J Applied Physiol. 2010;110:57–65.
Prado CM, Birdsell LA, Baracos VE. The emerging role of computerized tomography in assessing cancer cachexia. Curr Opin Support Palliat Care. 2009;3:269–75.
Harimoto N, Yoshizumi T, Shimokawa M, et al. Sarcopenia is a poor prognostic factor following hepatic resection in patients aged 70 years and older with hepatocellular carcinoma. Hepatol Res. 2016;46:1247–55.
Villasenor A, Ballard-Barbash R, Baumgartner K, et al. Prevalence and prognostic effect of sarcopenia in breast cancer survivors: the HEAL Study. J Cancer Surviv Res Pract. 2012;6:398–406.
Suzuki Y, Okamoto T, Fujishita T, et al. Clinical implications of sarcopenia in patients undergoing complete resection for early non-small cell lung cancer. Lung Cancer. 2016;101:92–7.
Kim EY, Kim YS, Park I, Ahn HK, Cho EK, Jeong YM. Prognostic significance of CT-determined sarcopenia in patients with small cell lung cancer. J Thorac Oncol. 2015;10:1795–9.
Prado CM, Lieffers JR, McCargar LJ, et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol. 2008;9:629–35.
Stene GB, Helbostad JL, Amundsen T, et al. Changes in skeletal muscle mass during palliative chemotherapy in patients with advanced lung cancer. Acta Oncol Stockh Sweden. 2015;54:340–8.
Rutten IJ, van Dijk DP, Kruitwagen RF, Beets-Tan RG, Olde Damink SW, van Gorp T. Loss of skeletal muscle during neoadjuvant chemotherapy is related to decreased survival in ovarian cancer patients. J Cachexia Sarcopenia Muscle. 2016;7:458–66.
Miyake M, Morizawa Y, Hori S, et al. Clinical impact of postoperative loss in psoas major muscle and nutrition index after radical cystectomy for patients with urothelial carcinoma of the bladder. BMC Cancer.2017;17:237.
Kawaguchi T, Takada M, Kubo A, et al. Performance status and smoking status are independent favorable prognostic factors for survival in non-small cell lung cancer: a comprehensive analysis of 26,957 patients with NSCLC. J Thorac Oncol. 2010;5:620–30.
Zengin A, Pye SR, Cook MJ, et al. Associations of muscle force, power, cross-sectional muscle area, and bone geometry in older UK men. J Cachexia Sarcopenia Muscle. 2017;8:598–606.
Reisinger KW, Bosmans JW, Uittenbogaart M, et al. Loss of skeletal muscle mass during neoadjuvant chemoradiotherapy predicts postoperative mortality in esophageal cancer surgery. Ann Surg Oncol. 2015;22:4445–52.
Hanai T, Shiraki M, Ohnishi S, et al. Rapid skeletal muscle wasting predicts worse survival in patients with liver cirrhosis. Hepatol Res. 2016;46:743–51.
Miyamoto Y, Baba Y, Sakamoto Y, et al. Negative impact of skeletal muscle loss after systemic chemotherapy in patients with unresectable colorectal cancer. PLoS ONE. 2015;10:e0129742.
Cao DX, Wu GH, Zhang B, et al. Resting energy expenditure and body composition in patients with newly detected cancer. Clin Nutr Edinburgh Scotland. 2010;29:72–7.
Kubo Y, Naito T, Mori K, Osawa G, Aruga E. Skeletal muscle loss and prognosis of breast cancer patients. Support Care Cancer. 2017;25:2221–2227.
Fukushima H, Nakanishi Y, Kataoka M, Tobisu KI, Koga F. Postoperative changes in skeletal muscle mass predict survival of patients with metastatic renal cell carcinoma undergoing cytoreductive nephrectomy. Clin Genitourin Cancer. 2016;15:e229–e238.
Ryu M, Jo J, Lee Y, Chung YS, Kim KM, Baek WC. Association of physical activity with sarcopenia and sarcopenic obesity in community-dwelling older adults: the Fourth Korea National Health and Nutrition Examination Survey. Age Ageing. 2013;42:734–40.
Bosaeus I, Rothenberg E. Nutrition and physical activity for the prevention and treatment of age-related sarcopenia. Proceed Nutr Soc. 2016;75:174–80.
Jaitovich A, Angulo M, Lecuona E, et al. High CO2 levels cause skeletal muscle atrophy via AMP-activated kinase (AMPK), FoxO3a protein, and muscle-specific Ring finger protein 1 (MuRF1). J Biol Chem. 2015;290:9183–94.
Jeon YK, Shin MJ, Kim MH, et al. Low pulmonary function is related with a high risk of sarcopenia in community-dwelling older adults: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008–2011. Osteoporosis Int. 2015;26:2423–9.
Bade BC, Thomas DD, Scott JB, Silvestri GA. Increasing physical activity and exercise in lung cancer: reviewing safety, benefits, and application. J Thorac Oncol. 2015;10:861–71.
Holden DA, Rice TW, Stelmach K, Meeker DP. Exercise testing, 6-min walk, and stair climb in the evaluation of patients at high risk for pulmonary resection. Chest. 1992;102:1774–9.
Woods JA, Davis JM, Kohut ML, Ghaffar A, Mayer EP, Pate RR. Effects of exercise on the immune response to cancer. Med Sci Sports Exerc. 1994;26:1109–15.
Woods JA, Davis JM, Smith JA, Nieman DC. Exercise and cellular innate immune function. Med Sci Sports Exercise. 1999;31:57–66.
Okita K, Nishijima H, Murakami T, et al. Can exercise training with weight loss lower serum C-reactive protein levels? Arterioscler Thrombosis Vasc Biol. 2004;24:1868–73.
Konig D, Deibert P, Winkler K, Berg A. Association between LDL-cholesterol, statin therapy, physical activity, and inflammatory markers in patients with stable coronary heart disease. Exercise Immunol Rev. 2005;11:97–107.
Mora S, Lee IM, Buring JE, Ridker PM. Association of physical activity and body mass index with novel and traditional cardiovascular biomarkers in women. JAMA. 2006;295:1412–9.
Temel JS, Abernethy AP, Currow DC, et al. Anamorelin in patients with non-small-cell lung cancer and cachexia (ROMANA 1 and ROMANA 2): results from two randomised, double-blind, phase 3 trials. Lancet Oncol. 2016;17:519–31.
Acknowledgment
We thank J. L. Croxford, PhD, and Alison Sherwin, PhD, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this report.
Disclosure
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10434_2017_6328_MOESM2_ESM.tiff
Electronic supplementary material 2 (TIFF 2788 kb) Supplementary Fig. 1 Detailed analyses of survival probabilities according to changes in skeletal muscle area (SMA) before and after surgery (approximately one year). All patients were classified into a ‘SMA-greatly decreased’ (post/pre ratio < 0.9), ‘SMA-slightly decreased’ (0.9 ≤ post/pre ratio ≤ 0.95), and ‘SMA-equal’ groups (post/pre ratio > 0.95). (a) The degree of poor disease-free survival depended on the extent of decrease in SMA (p = 0.003). (b) The degree of poor overall survival depended on the extent of the decrease in SMA (p = 0.004).
10434_2017_6328_MOESM3_ESM.tiff
Electronic supplementary material 3 (TIFF 2788 kb) Supplementary Fig. 2. Subgroup analysis of the change in normalized skeletal muscle area at the level of the 12th thoracic vertebrae before and after surgery (approximately 1 year) according to sex. (a) In men, the mean preoperative normalized skeletal muscle area was 12.33 cm2/m2, and decreased to 11.34 cm2/m2 (p = 0.047). (b) In women, the mean preoperative normalized skeletal muscle area was 11.22 cm2/m2, and decreased to 10.68 cm2/m2 postoperatively (p = 0.200).
Rights and permissions
About this article
Cite this article
Takamori, S., Toyokawa, G., Okamoto, T. et al. Clinical Impact and Risk Factors for Skeletal Muscle Loss After Complete Resection of Early Non-small Cell Lung Cancer. Ann Surg Oncol 25, 1229–1236 (2018). https://doi.org/10.1245/s10434-017-6328-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-6328-y