Abstract
Background
Open inguinal lymphadenectomy (OIL) has a high incidence of complications. The authors adapted and reported a minimally invasive technique [videoscopic inguinal lymphadenectomy (VIL)] for use with melanoma, subsequently pursuing a randomized, prospective trial comparing open and minimally invasive approaches in an attempt to confirm retrospective findings illustrating reduced complications with the minimally invasive approach.
Methods
A randomized, prospective trial (NCT01526486) was designed to compare outcomes for patients undergoing VIL versus OIL. Patients with a diagnosis of malignancies requiring inguinal lymphadenectomy at Emory University were enrolled in the study, and informed consent was obtained. Failure to accrue sufficient patients resulted in suspension of the randomization process. Clinicopathologic, procedural, and outcomes data on VILs were prospectively collected. The primary outcome was wound complications, and the secondary outcome was recurrence-free survival.
Results
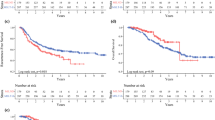
The results are limited to VILs. In this study, 102 patients underwent 137 procedures. Most of the complications were Clavien-Dindo 1 or 2, accounting for 89.7% of all postoperative issues. The wound infection rate was 47.4%. Skin necrosis or wound dehiscence occurred after 13 of the procedures (9.5%). For the patients with melanoma, the median overall survival was 68.8 months, and the recurrence-free survival was 18.5 months. The median inguinal recurrence-free survival was not reached. The median stage-specific recurrence-free survival was not reached for stage IIIA, was 22.8 months for stage IIIB, and was 8.8 months for stage IIIC disease (p < 0.001).
Conclusions
The long-term findings presented in this report expand on and confirm previously published results demonstrating decreased morbidity and oncologic noninferiority of VIL, further validating the technique for patients requiring lymphadenectomy.

Similar content being viewed by others
References
Balch CM, Soong SJ, Gershenwald JE, Thompson JF, Reintgen DS, Cascinelli N, et al. Prognostic factors analysis of 17,600 melanoma patients: validation of the American Joint Committee on Cancer Melanoma Staging System. J Clin Oncol. 2001;19:3622–34.
Srinivas V, Morse MJ, Herr HW, Sogani PC, Whitmore Jr WF. Penile cancer: relation of extent of nodal metastasis to survival. J Urol. 1987;137:880–2.
McMahon CJ, Rofsky NM, Pedrosa I. Lymphatic metastases from pelvic tumors: anatomic classification, characterization, and staging. Radiology. 2010;254:31–46.
Diller ML, Martin BM, Delman KA. Lymph node dissection for stage III melanoma. Surg Oncol Clin North Am. 2015; 24:261–77.
Morton DL, Thompson JF, Cochran AJ, Mozzillo N, Nieweg OE, Roses DF, et al. Final trial report of sentinel-node biopsy versus nodal observation in melanoma. N Engl J Med. 2014;370:599–609.
Bilimoria KY, Balch CM, Bentrem DJ, Talamonti MS, Ko CY, Lange JR, et al. Complete lymph node dissection for sentinel node-positive melanoma: assessment of practice patterns in the United States. Ann Surg Oncol. 2008;15:1566–76.
de Vries M, Hoekstra HJ, Hoekstra-Weebers JE. Quality of life after axillary or groin sentinel lymph node biopsy, with or without completion lymph node dissection, in patients with cutaneous melanoma. Ann Surg Oncol. 2009;16:2840–7.
Shaw JH, Rumball EM. Complications and local recurrence following lymphadenectomy. Br J Surg. 1990;77:760–4.
Poos HP, Kruijff S, Bastiaannet E, van Ginkel RJ, Hoekstra HJ. Therapeutic groin dissection for melanoma: risk factors for short-term morbidity. Eur J Surg Oncol. 2009;35:877–83.
Johnson TV, Hsiao W, Delman KA, Jani AB, Brawley OW, Master VA. Extensive inguinal lymphadenectomy improves overall 5-year survival in penile cancer patients: results from the surveillance, epidemiology, and end results program. Cancer. 2010;116:2960–6.
Stuiver MM, Westerduin E, Ter Meulen S, Vincent AD, Nieweg OE, Wouters MW. Surgical wound complications after groin dissection in melanoma patients: a historical cohort study and risk factor analysis. Eur J Surg Oncol. 2014;40:1284–90.
Stuiver MM, Djajadiningrat RS, Graafland NM, Vincent AD, Lucas C, Horenblas S. Early wound complications after inguinal lymphadenectomy in penile cancer: a historical cohort study and risk-factor analysis. Eur Urol. 2013;64:486–92.
Chang SB, Askew RL, Xing Y, Weaver S, Gershenwald JE, Lee JE. Prospective assessment of postoperative complications and associated costs following inguinal lymph node dissection (ILND) in melanoma patients. Ann Surg Oncol. 2010;17:2764–72.
Serpell JW, Carne PW, Bailey M. Radical lymph node dissection for melanoma. ANZ J Surg. 2003;73:294–9.
van Akkooi ACJ, Bouwhuis MG, Van Geel AN, Hoedemaker R, Verhoef C, Grunhagen DJ, et al. Morbidity and prognosis after therapeutic lymph node dissections for malignant melanoma. EJSO Eur J Surg Oncol. 2007;33:102–8.
Bowsher WG, Taylor BA, Hughes LE. Morbidity, mortality, and local recurrence following regional node dissection for melanoma. Br J Surg. 1986;73:906–8.
Slagelse C, Petersen KL, Dahl JB, Finnerup K, Greene K, Leong SP, et al. Persistent postoperative pain and sensory changes following lymph node excision in melanoma patients: a topical review. Melanoma Res. 2014;24:93–8.
Martin BM, Master VA, Delman KA. Minimizing morbidity in melanoma surgery. Oncology. 2013;27:1016–20.
Mortenson MM, et al. Fibrin sealant does not decrease seroma output or time to drain removal following inguino-femoral lymph node dissection in melanoma patients: a randomized controlled trial (NCT00506311). World J Surg Oncol. 2008;6:63.
Tobias-Machado M, Tavares A, Molina WR Jr, Zambon JP, Medina JA, Forseto Jr PH, et al. Video endoscopic inguinal lymphadenectomy (VEIL): initial case report and comparison with open radical procedure. Arch Esp Urol. 2006;59:849–52.
Romanelli P, Nishimoto R, Suarez R, Decia R, Abreu D, Machado M, et al. Video endoscopic inguinal lymphadenectomy: surgical and oncological results. Actas Urol Esp. 2013;37:305–10.
Delman KA, Kooby DA, Ogan K, Hsiao W, Master V. Feasibility of a novel approach to inguinal lymphadenectomy: minimally invasive groin dissection for melanoma. Ann Surg Oncol. 2010;17:731–7.
Delman KA, Kooby DA, Rizzo M, Ogan K, Master V. Initial experience with videoscopic inguinal lymphadenectomy. Ann Surg Oncol. 2011;18:977–82.
Sommariva A, Pasquali S, Rossi CR. Video endoscopic inguinal lymphadenectomy for lymph node metastasis from solid tumors. Eur J Surg Oncol. 2015;41:274–81.
Master V, Ogan K, Kooby D, Hsiao W, Delman K. Leg endoscopic groin lymphadenectomy (LEG procedure): step-by-step approach to a straightforward technique. Eur Urol. 2009;56:821–8.
Martin BM, tra JW, Russell MC, Rizzo M, Kooby DA, Staley CA, et al. Oncologic outcomes of patients undergoing videoscopic inguinal lymphadenectomy for metastatic melanoma. J Am Coll Surg. 2014;218:620–6.
Balch CM, Gershenwald JE, Soong SJ, Thompson JF, Atkins MB, Byrd DR, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009;27:6199–206.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Onaitis MW, Petersen RP, Balderson SS, Toloza E, Burfeind WR, Harpole Jr DH, et al. Thoracoscopic lobectomy is a safe and versatile procedure: experience with 500 consecutive patients. Ann Surg. 2006;244:420–5.
Frumovitz M, Dos Reis R, Sun CC, Milam MR, Bevers MW, Brown J, et al. Comparison of total laparoscopic and abdominal radical hysterectomy for patients with early-stage cervical cancer. Obstet Gynecol. 2007;110:96–102.
Puzziferri N, Austrheim-Smith IT, Wolfe BM, Wilson SE, Nguyen NT. Three-year follow-up of a prospective randomized trial comparing laparoscopic versus open gastric bypass. Ann Surg. 2006;243:181–8.
Spiess PE, Hernandez MS, Pettaway CA. Contemporary inguinal lymph node dissection: minimizing complications. World J Urol. 2009;27:205–12.
Beitsch P, Balch C. Operative morbidity and risk factor assessment in melanoma patients undergoing inguinal lymph node dissection. Am J Surg. 1992;164:462–5; discussion 465–6.
White RR, Stanley WE, Johnson JL, Tyler DS, Seigler HF. Long-term survival in 2505 patients with melanoma with regional lymph node metastasis. Ann Surg. 2002;235:879–87.
Lee DY, Lau BJ, Huynh KT, Flaherty DC, Lee JH, Stern SL, et al. Impact of completion lymph node dissection on patients with positive sentinel lymph node biopsy in melanoma. J Am Coll Surg. 2016;223:9–18.
Acknowledgment
This work was supported in part by the Winship Skin Cancer and Melanoma Fund, the Katz Foundation, and a Kennedy Seed Grant.
Disclosure
The authors have no relevant disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Postlewait, L.M., Farley, C.R., Diller, M.L. et al. A Minimally Invasive Approach for Inguinal Lymphadenectomy in Melanoma and Genitourinary Malignancy: Long-Term Outcomes in an Attempted Randomized Control Trial. Ann Surg Oncol 24, 3237–3244 (2017). https://doi.org/10.1245/s10434-017-5971-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-5971-7