Abstract
Background
The ACOSOG Z0011 (Z11) trial demonstrated that in patients with nonpalpable axillary lymph nodes (LN) and one to two positive sentinel LN (SLN), axillary LN dissection (ALND) is unnecessary.JAMA 305:569–575, [2011], Ann Surg 264:413–42, [2016] The Z11 trial did not require preoperative axillary ultrasound (axUS). In many centers, preoperative axUS is part of the standard workup of a newly diagnosed breast cancer patient, but in light of the Z11 results, its role is now questioned.
Methods
We retrospectively analyzed newly diagnosed breast cancer patients at two institutions. Inclusion criteria were patients with (1) no palpable lymphadenopathy, (2) abnormal axUS, (3) axillary LN metastasis confirmed preoperatively by axUS-lymph node needle biopsy, (4) no neoadjuvant therapy, and (5) ALND. LN disease burden was dichotomized as N1 versus N2-3. We examined relationships between clinicopathologic factors, including axUS characteristics, and LN disease burden.
Results
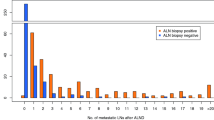
Of 129 included cases, 67 had N1 disease (51.9%) and 62 had N2-3 disease (48.1%). Factors significantly associated with N1 disease were tumor size ≤2 cm (p = 0.012), nonlobular histology (p = 0.013), and one suspicious LN on axUS (p = 0.008). For patients with both tumor size on imaging ≤2 cm and one abnormal LN on axUS, only 27% had N2-3 disease (p = 0.007).
Conclusions
More than half of patients without palpable adenopathy but with preoperative US-guided biopsy proven axillary LN metastases had N1 disease. For patients with both tumor size ≤2 cm and only 1 abnormal LN on axUS, 73% had N1 disease. This suggests that such patients, if they are otherwise analogous to Z11 patients, may undergo attempt at SLNB.

Similar content being viewed by others
References
Giuliano AE, Hunt KK, Ballman KV, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011;305(6):569–75.
Giuliano AE, Ballman K, McCall L, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: long-term follow-up from the american college of surgeons oncology group (alliance) ACOSOG Z0011 randomized trial. Ann Surg. 2016;264(3):413–20.
van Wely BJ, de Wilt JH, Francissen C, Teerenstra S, Strobbe LJ. Meta-analysis of ultrasound-guided biopsy of suspicious axillary lymph nodes in the selection of patients with extensive axillary tumour burden in breast cancer. Br J Surg. 2015;102(3):159–68.
Tahir M, Osman KA, Shabbir J, et al. Preoperative axillary staging in breast cancer-saving time and resources. Breast J. 2008;14(4):369–71.
van Rijk MC, Deurloo EE, Nieweg OE, et al. Ultrasonography and fine-needle aspiration cytology can spare breast cancer patients unnecessary sentinel lymph node biopsy. Ann Surg Oncol. 2006;13(1):31–5.
Reyna C, Kiluk JV, Frelick A, Khakpour N, Laronga C, Lee MC. Impact of axillary ultrasound (AUS) on axillary dissection in breast conserving surgery (BCS). J Surg Oncol. 2015;111(7):813–8.
Pilewskie M, Jochelson M, Gooch JC, Patil S, Stempel M, Morrow M. Is preoperative axillary imaging beneficial in identifying clinically node-negative patients requiring axillary lymph node dissection? J Am Coll Surg. 2016;222(2):138–45.
Pilewskie M, Mautner SK, Stempel M, Eaton A, Morrow M. Does a positive axillary lymph node needle biopsy result predict the need for an axillary lymph node dissection in clinically node-negative breast cancer patients in the ACOSOG Z0011 era? Ann Surg Oncol. 2016;23(4):1123–8.
Boughey JC, Ballman KV, Hunt KK, et al. Axillary ultrasound after neoadjuvant chemotherapy and its impact on sentinel lymph node surgery: results from the American College of Surgeons Oncology group Z1071 trial (alliance). J Clin Oncol. 2015;33(30):3386–93.
Kuru B, Gulcelik MA, Topgul K, et al. Application of sentinel node biopsy in breast cancer patients with clinically negative and positive axilla and role of axillary ultrasound examination to select patients for sentinel node biopsy. J BUON. 2011;16(3):454–9.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Harris, C.K., Tran, H.T., Lee, K. et al. Positive Ultrasound-guided Lymph Node Needle Biopsy in Breast Cancer may not Mandate Axillary Lymph Node Dissection. Ann Surg Oncol 24, 3004–3010 (2017). https://doi.org/10.1245/s10434-017-5935-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-5935-y