Abstract
Background
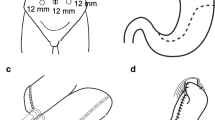
A novel double-flap esophagogastrostomy technique developed to prevent reflux after proximal gastrectomy was applied to laparoscopic proximal gastrectomy (LPG), and the clinical outcomes of this technique (LPG-DFT) were evaluated and compared to those of laparoscopic total gastrectomy (LTG).
Methods
This retrospective study of 90 patients with early gastric cancer (EGC) in the upper third of the stomach compared surgical outcomes, postoperative endoscopic findings, and nutritional status between two procedure groups, LPG-DFT (n = 43) and LTG (n = 47). The association between morbidity and surgical procedure was analyzed by controlling for body mass index (BMI).
Results
Mean operation time was significantly higher for LPG-DFT than LTG (386.5 vs. 316.3 min, P < 0.001). The morbidity and the frequency of anastomotic complications were lower, although not significantly, for LPG-DFT than LTG (7.0 vs. 21.3%, P = 0.073; and 4.7 vs. 17.2%, P = 0.093). Median postoperative hospital stay was significantly shorter for LPG-DFT than LTG (10 vs. 13 days, P = 0.002). The LPG-DFT procedure was identified as the most significant independent predictor of low morbidity after adjustment for BMI (P = 0.028, OR = 0.232, 95% CI 0.047–0.862). LTG induced more severe reflux esophagitis than LPG-DFT (14.9% vs. 2.3%, P = 0.06). The mean baseline weight, total protein, and hemoglobin were significantly higher with LPG-DFT than with LTG (P < 0.05).
Conclusions
LPG-DFT is a better surgical procedure for treating upper-third EGC than LTG in terms of morbidity, postoperative hospital stay, and postoperative nutritional status.


Similar content being viewed by others
Change history
17 May 2018
In the original article on page 1636, first line, the reference cited for Kamikawa et al. is incorrect. The correct reference is as follows: Kamikawa YKT, Kamiyama S, Satomoto K. A new procedure of esophagogastrostomy to prevent reflux following proximal gastrectomy (in Japanese). Shoukakigeka. 2001;24:1053–60.
17 May 2018
In the original article on page 1636, first line, the reference cited for Kamikawa et al. is incorrect. The correct reference is as follows: Kamikawa Y, Kobayashi T, Kamiyama S, et al. A new procedure of esophagogastrostomy to prevent reflux following proximal gastrectomy (in Japanese). Shoukakigeka. 2001;24:1053?60.
17 May 2018
In the original article on page 1636, first line, the reference cited for Kamikawa et al. is incorrect. The correct reference is as follows: Kamikawa Y, Kobayashi T, Kamiyama S, et al. A new procedure of esophagogastrostomy to prevent reflux following proximal gastrectomy (in Japanese). Shoukakigeka. 2001;24:1053?60.
References
Ahn HS, Lee HJ, Yoo MW, et al. Changes in clinicopathological features and survival after gastrectomy for gastric cancer over a 20-year period. Br J Surg. 2011;98(2):255–60.
Blaser MJ, Saito D. Trends in reported adenocarcinomas of the oesophagus and gastric cardia in Japan. Eur Gastroenterol Hepatol. 2002;14(2):107–13.
Isobe Y, Nashimoto A, Akazawa K, et al. Gastric cancer treatment in Japan: 2008 annual report of the JGCA nationwide registry. Gastric Cancer: Off J Int Gastric Cancer Assoc Japanese Gastric Cancer Assoc. 2011;14(4):301–16.
Jang JH, Beron RI, Ahn HS, et al. Clinicopathological features of upper third gastric cancer during a 21-year period (single center analysis). J Gastric Cancer. 2010;10(4):212–8.
Katai H, Sano T, Fukagawa T, Shinohara H, Sasako M. Prospective study of proximal gastrectomy for early gastric cancer in the upper third of the stomach. Br J Surg. 2003;90(7):850–3.
Zhou Y, Zhang Z, Zhang Z, et al. A rising trend of gastric cardia cancer in Gansu Province of China. Cancer Lett. 2008;269(1):18–25.
An JY, Youn HG, Choi MG, Noh JH, Sohn TS, Kim S. The difficult choice between total and proximal gastrectomy in proximal early gastric cancer. Am J Surg. 2008;196(4):587–91.
Seshimo A, Miyake K, Amano K, Aratake K, Kameoka S. Clinical outcome of esophagogastrostomy after proximal gastrectomy for gastric cancer. Hepatogastroenterology. 2013;60(123):616–9.
Ronellenfitsch U, Najmeh S, Andalib A, et al. Functional outcomes and quality of life after proximal gastrectomy with esophagogastrostomy using a narrow gastric conduit. Ann Surg Oncol. 2015;22(3):772–9.
Tokunaga M, Ohyama S, Hiki N, et al. Endoscopic evaluation of reflux esophagitis after proximal gastrectomy: comparison between esophagogastric anastomosis and jejunal interposition. World J Surg. 2008;32(7):1473–7.
Nomura E, Lee SW, Kawai M, et al. Functional outcomes by reconstruction technique following laparoscopic proximal gastrectomy for gastric cancer: double tract versus jejunal interposition. World J Surg Oncol. 2014;12:20.
Ahn SH, Jung do H, Son SY, Lee CM, Park do J, Kim HH. Laparoscopic double-tract proximal gastrectomy for proximal early gastric cancer. Gastric Cancer. 2014;17(3):562–70.
Fukagawa T, Gotoda T, Oda I, et al. Stenosis of esophago-jejuno anastomosis after gastric surgery. World J. Surg. 2010;34(8):1859–63.
Kuroda S, Nishizaki M, Kikuchi S, et al. Double flap technique as an anti-reflux procedure in esophagogastrostomy after proximal gastrectomy. J. Am. Coll. Surg. May 5 2016.
Muraoka A, Kobayashi M, Kokudo Y. Laparoscopy-assisted proximal gastrectomy with the hinged double flap method. World J Surg Apr 19 2016.
Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer: Off J Int Gastric Cancer Assoc Japanese Gastric Cancer Assoc. 2011;14(2):101–12.
Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer: Off J Int Gastric Cancer Assoc Japanese Gastric Cancer Assoc. 2011;14(2):113–23.
Mine S, Nunobe S, Watanabe M. A Novel Technique of Anti-reflux Esophagogastrostomy Following Left Thoracoabdominal Esophagectomy for Carcinoma of the Esophagogastric Junction. World J Surg. Apr 23 2015.
Nunobe S, Hiki N, Tanimura S, et al. Three-step esophagojejunal anastomosis with atraumatic anvil insertion technique after laparoscopic total gastrectomy. J Gastrointest Surg. 2011;15(9):1520–5.
Kosuga T, Hiki N, Nunobe S, et al. Does the Single-stapling technique for circular-stapled esophagojejunostomy reduce anastomotic complications after laparoscopic total gastrectomy? Ann Surg Oncol. 2015;22(11):3606–12.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Lee SW, Kawai M, Tashiro K, et al. Laparoscopic gastrointestinal anastomoses using knotless barbed absorbable sutures are safe and reproducible: a single-center experience with 242 patients. Jpn J Clin Oncol. 2016;46(4):329–35.
Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature. 402(6762):656–60.
Takiguchi S, Hiura Y, Miyazaki Y, Takata A, Murakami K, Doki Y. Clinical trial of ghrelin synthesis administration for upper GI surgery. Methods Enzymol. 2012;514:409–31.
Lim CH, Kim SW, Kim WC, et al. Anemia after gastrectomy for early gastric cancer: long-term follow-up observational study. World J Gastroenterol. 18(42):6114–9.
Takiguchi N, Takahashi M, Ikeda M, et al. Long-term quality-of-life comparison of total gastrectomy and proximal gastrectomy by postgastrectomy syndrome assessment scale (PGSAS-45): a nationwide multi-institutional study. Gastric Cancer: Off J Int Gastric Cancer Assoc Japanese Gastric Cancer Assoc. 18(2):407–16.
Acknowledgement
The authors would like to thank Dr. Naoki Ishizuka for his statistical advice and for always taking the time to read this manuscript and respond rapidly with valuable suggestions for improvements.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hayami, M., Hiki, N., Nunobe, S. et al. Clinical Outcomes and Evaluation of Laparoscopic Proximal Gastrectomy with Double-Flap Technique for Early Gastric Cancer in the Upper Third of the Stomach. Ann Surg Oncol 24, 1635–1642 (2017). https://doi.org/10.1245/s10434-017-5782-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-5782-x