Abstract
Background
Reactive oxygen species (ROS) generated by chemoradiotherapy lead to cancer cell death. Although ROS regulation mechanisms play important roles in chemoradioresistance, few markers exist that indicated intracellular ROS status. This study aimed to identify novel cell surface markers that represented intracellular ROS status to characterize cells with low ROS (ROSlow) in colorectal cancer (CRC).
Methods
We used ROS indicators and an antibody array with 242 cell surface antibodies to identify markers of ROSlow cells. After validation, we performed immunohistochemical analyses and chemosensitivity assays. We used small interfering RNA to assess the effect of silencing the identified markers. We tested cell differentiation assays with spheroid cell assays.
Results
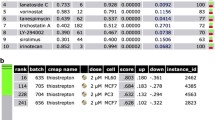
CD107a was identified as a common marker of ROSlow cells in several CRC cell lines and clinical specimens. CD107a+/ROSlow cells were enriched in HT29 and DLD1 cultures after treatments with oxaliplatin, 5-fluorouracil, and the irinotecan metabolite SN38. CD107a silencing improved chemosensitivity by increasing ROS production. Immunohistochemistry showed enhanced CD107a surface expression on cells that formed immature cell clusters and on cells located in the invasive fronts of cancer foci. CD107a expression was also enhanced on specimens from patients with poorly differentiated adenocarcinoma who had received neoadjuvant chemotherapy. Cell surface CD107a expression was enhanced on cells that formed colonospheres, but expression diminished during cell differentiation.
Conclusions
CD107a was identified as a novel marker of ROSlow cells in CRC. CD107a expression was closely related to chemoresistance and the immature cell phenotype. Anti-CD107a treatments represent a novel approach for targeting chemoresistant cells in CRC.





Similar content being viewed by others
References
Uehara K, Nagano M. Neoadjuvant treatment for locally advanced rectal cancer: a systematic review. Surg Today. 2016;46:161–8.
Okuma H, Uchikado Y, Setoyama T, Matsumoto M, Owaki T, Ishigami S, et al. Biomarkers for predicting the response of esophageal squamous cell carcinoma to neoadjuvant chemoradiation therapy. Surg Today. 2014;44:421–8.
Hsiang YH, Lihou MG, Liu LF. Arrest of replication forks by drug-stabilized topoisomerase I—DNA cleavable complexes as a mechanism of cell killing by camptothecin. Cancer Res. 1989;49:5077–82.
Donaldson KL, Goolsby GL, Wahl AF. Cytotoxicity of the anticancer agents cisplatin and Taxol during cell proliferation and the cell cycle. Int J Cancer. 1994;57:847–55.
Ozben T. Oxidative stress and apoptosis: impact on cancer therapy. J Pharm Sci. 2007;96:2181–96.
Kaufmann SH, Earnshaw WC. Induction of apoptosis by cancer chemotherapy. Exp Cell Res. 2000;256:42–9.
Li X, Zhu F, Jiang J, Sun C, Wang X, Shen M, et al. Synergistic antitumor activity of withaferin A combined with oxaliplatin triggers reactive oxygen species–mediated inactivation of the PI3K/AKT pathway in human pancreatic cancer cells. Cancer Lett. 2015;357:219–30.
Xing Y, Bao W, Fan X, Liu K, Li X, Xi T. A novel oxaliplatin derivative, Ht-2, triggers mitochondrion-dependent apoptosis in human colon cancer cells. Apoptosis. 2015;20:83–91.
Szatrowski TP, Nathan CF. Production of large amounts of hydrogen peroxide by human tumor cells. Cancer Res. 1991;51:794–8.
Haraguchi N, Ishii H, Mimori K, Tanaka F, Ohkuma M, Kim HM, et al. CD13 is a therapeutic target in human liver cancer stem cells. J Clin Invest. 2010;120:3326–39.
Kim HM, Haraguchi N, Ishii H, Ohkuma M, Okano M, Mimori K, et al. Increased CD13 expression reduces reactive oxygen species, promoting survival of liver cancer stem cells via an epithelial–mesenchymal transition–like phenomenon. Ann Surg Oncol. 2012;19: 39–48.
Diehn M, Cho RW, Lobo NA, Kalisky T, Dorie MJ, Kulp AN, et al. Association of reactive oxygen species levels and radioresistance in cancer stem cells. Nature. 2009;458:780–3.
Ishimoto T, Nagano O, Yae T, Tamada M, Motohara T, Oshima H, et al. CD44 variant regulates redox status in cancer cells by stabilizing the xCT subunit of system xc- and thereby promotes tumor growth. Cancer Cell. 2011;19:387–400.
Song IS, Jeong YJ, Jeong SH, Heo HJ, Kim HK, Bae KB, et al. FOXM1-induced PRX3 regulates stemness and survival of colon cancer cells via maintenance of mitochondrial function. Gastroenterology. 2015;149:1006–16.
Moore KA, Lemischka IR. Stem cells and their niches. Science. 2006;311:1880–5.
Naka K, Muraguchi T, Hoshii T, Hirao A. Regulation of reactive oxygen species and genomic stability in hematopoietic stem cells. Antioxid Redox Signal. 2008;10:1883–94.
Hosokawa K, Arai F, Yoshihara H, Nakamura Y, Gomei Y, Iwasaki H, et al. Function of oxidative stress in the regulation of hematopoietic stem cell–niche interaction. Biochem Biophys Res Commun. 2007;363:578–83.
Reisher SR, Hughes TE, Ordovas JM, Schaefer EJ, Feinstein SI. Increased expression of apolipoprotein genes accompanies differentiation in the intestinal cell line Caco-2. Proc Natl Acad Sci USA. 1993;90:5757–61.
Augeron C, Laboisse CL. Emergence of permanently differentiated cell clones in a human colonic cancer cell line in culture after treatment with sodium butyrate. Cancer Res. 1984;44:3961–9.
Sussman NL, Eliakim R, Rubin D, Perlmutter DH, DeSchryver-Kecskemeti K, Alpers DH. Intestinal alkaline phosphatase is secreted bidirectionally from villous enterocytes. Am J Physiol. 1989;257:G14–23.
Haraguchi N, Ohkuma M, Sakashita H, Matsuzaki S, Tanaka F, Mimori K, et al. CD133+CD44+ population efficiently enriches colon cancer initiating cells. Ann Surg Oncol. 2008;15:2927–33.
Ricci-Vitiani L, Lombardi DG, Pilozzi E, Biffoni M, Todaro M, Peschle C, et al. Identification and expansion of human colon-cancer-initiating cells. Nature. 2007;7123:111–5.
Vermeulen L, Todaro M, de Sousa Mello F, Sprick MR, Kemper K, Alea MP, et al. Single-cell cloning of colon cancer stem cells reveals a multi-lineage differentiation capacity. Proc Natl Acad Sci USA. 2008;105:13427–32.
Wei B, Han XY, Qi CL, Zhang S, Zheng ZH, Huang Y, et al. Coaction of spheroid-derived stem-like cells and endothelial progenitor cells promotes development of colon cancer. PLoS ONE. 2012;7:e39069.
Krzewski K, Gil-Krzewska A, Nguyen V, Peruzzi G, Coligan JE. LAMP1/CD107a is required for efficient perforin delivery to lytic granules and NK-cell cytotoxicity. Blood. 2013;121:4672–83.
Künzli BM, Berberat PO, Zhu ZW, Martignoni M, Kleeff J, Tempia‐Caliera AA, et al. Influences of the lysosomal associated membrane proteins (Lamp-1, Lamp-2) and Mac-2 binding protein (Mac-2-BP) on the prognosis of pancreatic carcinoma. Cancer. 2002;9:228–39.
Agarwal AK, Srinivasan N, Godbole R, More SK, Budnar S, Gude R, et al. Role of tumor cell surface lysosome-associated membrane protein-1 (LAMP1) and its associated carbohydrates in lung metastasis. J Cancer Res Clin Oncol. 2015;141:1563–74.
Eskelinen EL. Roles of LAMP-1 and LAMP-2 in lysosome biogenesis and autophagy. Mol Aspects Med. 2006;27:495–502.
Shi Y, Tang B, Yu PW, Tang B, Hao YX, Lei X, et al. Autophagy protects against oxaliplatin-induced cell death via ER stress and ROS in Caco-2 cells. PLoS ONE. 2012;7:e51076.
Ding ZB, Hui B, Shi YH, Zhou J, Peng YF, Gu CY, et al. Autophagy activation in hepatocellular carcinoma contributes to the tolerance of oxaliplatin via reactive oxygen species modulation. Clin Cancer Res. 2011;17:6229–38.
Sukhai MA, Prabha S, Hurren R, Rutledge AC, Lee AY, Sriskanthadevan S, et al. Lysosomal disruption preferentially targets acute myeloid leukemia cells and progenitors. J Clin Invest. 2013;123:315–28.
Jensen SS, Aaberg-Jessen C, Christensen KG, Kristensen B. Expression of the lysosomal-associated membrane protein-1 (LAMP-1) in astrocytomas. Int J Clin Exp Pathol. 2013;6:1294–305.
Todaro M, Francipaane MG, Medema JP, Stassi G. Colon cancer stem cells: promise of targeted therapy. Gastroenterology. 2010;138:2151–62.
Vaiopoulos AG, Kostakis ID, Koutsilieris M, Papavassiliou AG. Colorectal cancer stem cells. Stem Cells. 2012;30:363–71.
Huang AF, Chen MW, Huang SM, Kao CL, Lai HC, Chan JY. CD164 regulates the tumorigenesis of ovarian surface epithelial cells through the SDF-1α/CXCR4 axis. Mol Cancer. 2013;12:115.
Tang J, Zhang L, She X, Zhou G, Yu F, Xiang J, et al. Inhibiting CD164 expression in colon cancer cell line HCT116 leads to reduced cancer cell proliferation, mobility, and metastasis in vitro and in vivo. Cancer Invest. 2012;5:380–9.
Acknowledgement
Supported in part by the Foundation of the Pharma-Link between Academia and Shionogi (FLASH), an initiative between Osaka University and Shionogi & Co. Ltd.
Disclosure
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Tomohiro Kitahara and Naotsugu Haraguchi contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kitahara, T., Haraguchi, N., Takahashi, H. et al. Identification and Characterization of CD107a as a Marker of Low Reactive Oxygen Species in Chemoresistant Cells in Colorectal Cancer. Ann Surg Oncol 24, 1110–1119 (2017). https://doi.org/10.1245/s10434-016-5671-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5671-8