Abstract
Background
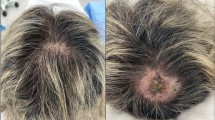
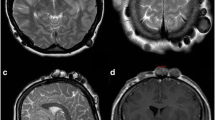
Scalp and neck melanomas (SNMs) have a relatively poor prognosis compared to other sites, and represent an anatomically challenging area for detection. The aim of this study was to identify the role of the hairdresser in detection of SNMs.
Methods
A tertiary surgical oncology institutional database was retrospectively reviewed for all patients undergoing resection of a scalp, posterior neck, or retro auricular invasive primary melanoma between 2008 and 2014.
Results
SNMs accounted for 128 melanoma patients during the study period, with median age 66 years, 88 % male, and median Breslow thickness 1.55 mm. Hairdressers detected 10 % of all SNMs, with hairdresser-detected SNMs presenting 13 years younger (53 vs. 66 years, P = 0.015), and with a trend towards lower Breslow depth (1.15 vs. 1.63) and more frequent discovery in AJCC Stage Ia or Ib (66.7 % vs. 44.8 %) than otherwise-detected SNMs. Women with SNMs were 1.8-fold more likely than men to have their SNMs detected by a hairdresser (P = 0.001), and presented at higher AJCC clinical stage than men and required wider surgical resection margins (P = 0.011). Women with hairdresser-detected SNMs were younger, with lower Breslow thickness and lower AJCC Clinical Stage than women with otherwise-detected SNM.
Conclusion
This study suggests that hairdressers play a critical role in detection of invasive primary scalp and neck melanoma, accounting for 10 % of all melanomas referred to a tertiary surgical oncology center. Quality improvement initiatives aimed at increasing early detection of scalp and neck melanoma should include members of the cosmetology community.

Similar content being viewed by others
References
Lachiewicz AM, Berwick M, Wiggins CL, Thomas NE. Survival differences between patients with scalp or neck melanoma and those with melanoma of other sites in the surveillance, epidemiology, and end results (SEER) program. Arch Dermatol. 2008;144(4):515–21.
de Giorgi V, Rossari S, Gori A, et al. The prognostic impact of the anatomical sites in the ‘head and neck melanoma’: scalp versus face and neck. Melanoma Res. 2012;22(5):402–5.
Benmeir P, Baruchin A, Lusthaus S, et al. Melanoma of the scalp: the invisible killer. Plast Reconstr Surg. 1995;95(3):496–500.
Shumate CR, Carlson GW, Giacco GG, Guinee VF, Byers RM. The prognostic implications of location for scalp melanoma. Am J Surg. 1991;162(4):315–9.
Roosta N, Black DS, Wong MK, Woodley DT. Assessing hairdressers’ knowledge of scalp and neck melanoma and their willingness to detect lesions and make referrals to dermatologists. J Am Acad Dermatol. 2013;68(1):183–5.
Bailey EE, Marghoob AA, Orengo IF, Testa MA, White VR, Geller AC. Skin cancer knowledge, attitudes, and behaviors in the salon: a survey of working hair professionals in Houston, Texas. Arch Dermatol. 2011;147(10):1159–65.
Turrisi R, Gunn H, Hultgren B, Warner N, Mallett KA. The style project: feasibility of collaborating with salons for prevention and early detection of skin cancer. Arch Dermatol. 2012;148(10):1206–7.
Pillemer BB, Pugliano-Mauro MA, Ferris LK, Patton TJ. Three cases of scalp melanomas discovered by hairdressers. J Clin Aesthet Dermatol. 2013;6(8):32–4.
Koh HK, Miller DR, Geller AC, Clapp RW, Mercer MB, Lew RA. Who discovers melanoma? Patterns from a population-based survey. J Am Acad Dermatol. 1992;26(6):914–9.
Linnan LA, Kim AE, Wasilewski Y, Lee AM, Yang J, Solomon F. Working with licensed cosmetologists to promote health: results from the North Carolina BEAUTY and health pilot study. Prev Med. 2001;33(6):606–12.
Solomon FM, Linnan LA, Wasilewski Y, Lee AM, Katz ML, Yang J. Observational study in ten beauty salons: results informing development of the North Carolina BEAUTY and health project. Health Educ. Behav. 2004;31(6):790–807.
Linnan LA, D’Angelo H, Harrington CB. A literature synthesis of health promotion research in salons and barbershops. Am J Prev Med. 2014;47(1):77–85.
Cox NH, Aitchison TC, Sirel JM, MacKie RM. Comparison between lentigo maligna melanoma and other histogenetic types of malignant melanoma of the head and neck. Scottish Melanoma Group. Br J Cancer. 1996;73(7):940–44.
Lesage C, Barbe C, Le Clainche A, Lesage FX, Bernard P, Grange F. Sex-related location of head and neck melanoma strongly argues for a major role of sun exposure in cars and photoprotection by hair. J Invest Dermatol. 2013;133(5):1205–11.
Golger A, Young DS, Ghazarian D, Neligan PC. Epidemiological features and prognostic factors of cutaneous head and neck melanoma: a population-based study. Arch Otolaryngol Head Neck Surg. 2007;133(5):442–7.
Green AC, Kimlin M, Siskind V, Whiteman DC. Hypothesis: hair cover can protect against invasive melanoma on the head and neck (Australia). Cancer Causes Control. 2006;17(10):1263–6.
Allen JD, Stoddard AM, Mays J, Sorensen G. Promoting breast and cervical cancer screening at the workplace: results from the woman to woman study. Am. J Public Health. 2001;91(4):584–90.
Holt CL, Wynn TA, Southward P, Litaker MS, Jeames S, Schulz E. Development of a spiritually based educational intervention to increase informed decision making for prostate cancer screening among church-attending African American men. J Health Commun. 2009;14(6):590–604.
Kreuter MW, Alcaraz KI, Pfeiffer D, Christopher K. Using dissemination research to identify optimal community settings for tailored breast cancer information kiosks. J Public Health Manag Pract. 2008;14(2):160–9.
Sadler GR, Ko CM, Cohn JA, White M, Weldon RN, Wu P. Breast cancer knowledge, attitudes, and screening behaviors among African American women: the Black cosmetologists promoting health program. BMC Public Health. 2007;7:57.
21. Sadler GR, Peterson M, Wasserman L, et al. Recruiting research participants at community education sites. J Cancer Educ. 2005;20(4):235–9.
Edwards BK, Brown ML, Wingo PA, et al. Annual report to the nation on the status of cancer, 1975-2002, featuring population-based trends in cancer treatment. J Natl Cancer Inst. 2005;97(19):1407–27.
Girardi S, Gaudy C, Gouvernet J, Teston J, Richard MA, Grob JJ. Superiority of a cognitive education with photographs over ABCD criteria in the education of the general population to the early detection of melanoma: a randomized study. Int J Cancer. 2006;118(9):2276–80.
Hall HI, Jamison P, Fulton JP, Clutter G, Roffers S, Parrish P. Reporting cutaneous melanoma to cancer registries in the United States. J Am Acad Dermatol. 2003;49(4):624–30.
Acknowledgment
Presented as a poster at the 2015 Society of Surgical Oncology Annual Cancer Symposium at Houston, Texas, March 2015.
Disclosures and Funding Sources
None to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lovasik, B.P., Sharma, I., Russell, M.C. et al. Invasive Scalp Melanoma: Role for Enhanced Detection Through Professional Training. Ann Surg Oncol 23, 4049–4057 (2016). https://doi.org/10.1245/s10434-016-5334-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5334-9