Abstract
Background
Current guidelines recommend the evaluation of at least 12 lymph nodes (LNs) in the pathologic specimen following surgery for colorectal cancer (CRC). We sought to examine the role of colorectal specialization on nodal identification.
Methods
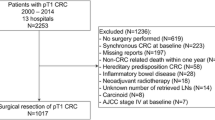
We conducted a retrospective cohort study using SEER-Medicare data to examine the association between colorectal specialization and LN identification following surgery for colon and rectal adenocarcinoma between 2001 and 2009. Our dataset included patients >65 years who underwent surgical resection for CRC. We excluded patients with rectal cancer who had received neoadjuvant therapy. The primary outcome measure was the number of LNs identified in the pathologic specimen following surgery for CRC. Multivariate analysis was used to identify the association between surgical specialization and LN identification in the pathologic specimen.
Results
In multivariate analysis, odds of an adequate lymphadenectomy following surgery with a colorectal specialist were 1.32 and 1.41 times greater for colon and rectal cancer, respectively, than following surgery by a general surgeon (p < 0.001). These odds increased to 1.36 and 1.58, respectively, when analysis was limited to board-certified colorectal surgeons. Hospital factors associated with ≥12 LNs identified included high-volume CRC surgery (colon OR 1.84, p < 0.001; rectal OR 1.78, p < 0.001) and NCI-designated Cancer Centers (colon OR 1.75, p < 0.001; rectal OR 1.64; p = 0.007).
Conclusions
Colorectal specialization and, in particular, board-certification in colorectal surgery, is significantly associated with increased LN identification following surgery for colon and rectal adenocarcinoma since the adoption of the 12-LN guideline in 2001.


Similar content being viewed by others
References
Howlader N, Noone AM, Krapcho M, et al. SEER cancer statistics review, 1975–2011. National Cancer Institute, Bethesda. http://seer.cancer.gov/csr/1975_2011/ (Based on November 2013 SEER data submission, posted to the SEER web site). Accessed Apr 2014.
Heald RJ, Ryall RD. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet. 1986;327:1479–82.
Enker WE, Thaler HT, Cranor ML, Polyak T. Total mesorectal excision in the operative treatment of carcinoma of the rectum. J Am Coll Surg. 1995;181(4):335–46.
Chang GJ, Rodriguez-Bigas MA, Skibber JM, Moyer VA. Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst. 2007;99(6):433–41.
Chen SL, Bilchik AJ. More extensive nodal dissection improves survival for stages I to III of colon cancer: a population-based study. Ann Surg. 2006;244(4):602–10.
Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ, Haller DG. Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol. 2003;21(15):2912–9.
Nelson H, Petrelli N, Carlin A, et al. Guidelines 2000 for colon and rectal cancer surgery. J Natl Cancer Inst. 2001;93:583–96.
Parsons HM, Tuttle TM, Kuntz KM, Begun JW, McGovern PM, Virnig BA. Association between lymph node evaluation for colon cancer and node positivity over the past 20 years. JAMA. 2011;306:1089–97.
Nathan H, Shore AD, Anders RA, Wick EC, Gearhart SL, Pawlik TM. Variation in lymph node assessment after colon cancer resection: patient, surgeon, pathologist, or hospital? J Gastrointest Surg. 2011;15:471–9.
Barbas A, Turley R, Mantyh C, Migaly J. Advanced fellowship training is associated with improved lymph node retrieval in colon cancer resections. J Surg Res. 2011;170:e41–6.
Nicholl MB, Wright BE, Conway WC, Aarnes-Leong T, Sim MS, Faries MB. Does specialized surgical training increase lymph node yield in colon cancer? Am Surg. 2009;10:887–91.
Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care. 2002;40(8):3–18.
Wichmann MW, Müller C, Meyer G, et al. Effect of preoperative radiochemotherapy on lymph node retrieval after resection of rectal cancer. Arch Surg. 2002;137(2):206–10.
Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53(12):1258–67.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Bilimoria KY, Bentrem DJ, Stewart AK, Talamonti MS, Winchester DP, Russell TR, Ko CY. Lymph node evaluation as a colon cancer quality measure: a national hospital report card. J Natl Cancer Inst. 2008;100(18):1310–7.
Parsons HM, Begun JW, McGovern PM, Tuttle TM, Kuntz KM, Virnig BA. Hospital characteristics associated with maintenance or improvement of guideline-recommended lymph node evaluation for colon cancer. Med Care. 2013;51(1):60–7.
Waters JA, Chihara R, Moreno J. Laparoscopic colectomy: does the learning curve extend beyond colorectal surgery fellowship? JSLS. 2010;14:325–31.
West NP, Hohenberger W, Weber K, Perrakis A, Finan PJ, Quirke P. Complete mesocolic excision with central vascular ligation produces an oncologically superior specimen compared with standard surgery for carcinoma of the colon. J Clin Oncol. 2009; 28:272–8.
Quirke P, Steele R, Monson J, et al. Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet. 2009;373(9666):821–8.
Monson JR, Probst CP, Wexner SD, et al. Failure of evidence-based cancer care in the United States: the association between rectal cancer treatment, cancer center volume, and geography. Ann Surg. 2014;260(4):625–31.
Author Contributions
Study concept and design: E.C.P. and S.S.; acquisition, analysis, and interpretation of data: all authors; drafting of manuscript: E.C.P. and A.N.J.; critical revision of manuscript for intellectual content: all authors; statistical analysis: E.C.P.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jeganathan, A.N., Shanmugan, S., Bleier, J.I.S. et al. Colorectal Specialization Increases Lymph Node Yield: Evidence from a National Database. Ann Surg Oncol 23, 2258–2265 (2016). https://doi.org/10.1245/s10434-016-5122-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5122-6