Abstract
Background
Although efficient chemotherapy regimens have improved outcomes after R1 resection (positive margins) for colorectal liver metastases (CLMs), the long-term survival benefit and potential for cure after R1 resection have not been clearly demonstrated. The aim of this study was to evaluate the long-term outcome after R1 resection for CLM, and to identify factors predictive of cure.
Methods
All resected CLM patients at our institution from 2000 to 2009 were prospectively evaluated. Cure was defined as a disease-free interval ≥5 years from the last hepatic or extrahepatic resection to last follow-up.
Results
Of 628 patients consecutively resected for CLM, 428 were eligible for the study, of whom 219 (51 %) underwent R0 resection (negative margins) and 209 (49 %) underwent R1 resection. Overall, 130 patients with R0 resection and 141 patients with R1 resection had more than 5 years of follow-up. Five- and 10-year overall survival rates were 56 and 34 % for R0 patients, and 48 and 36 % for R1 patients, respectively (p = 0.37). Of the 141 patients who underwent R1 resection, 26 patients (18 %) were considered ‘cured’, and 106 patients (75 %) were considered ‘noncured’. Independent predictive factors of cure after R1 resection included ≤10 total cycles of preoperative chemotherapy and objective response to preoperative chemotherapy.
Conclusions
Overall, potential cure can be achieved in 18 % of patients after R1 resection for CLM. The best conditions to achieve long-term survival after R1 resection rely on a good response to efficient and short first-line chemotherapy.



Similar content being viewed by others
References
de Hass RJ, Wicherts DA, Flores E, et al. R1 resection by necessity for colorectal liver metastases: is it still a contraindication to surgery? Ann Surg. 2008;248:626–37.
Ekberg H, Tranberg KG, Andersson R, et al. Determinants of survival in liver resection for colorectal secondaries. Br J Surg. 1986;73:727–31.
Shirabe K, Takenaka K, Gion T, et al. Analysis of prognostic risk factors in hepatic resection for metastatic colorectal carcinoma with special reference to the surgical margin. Br J Surg. 1997;84:1077–80.
Cady B, Jenkins RL, Steele GD Jr, et al. Surgical margin in hepatic resection for colorectal metastasis: a critical and improvable determinant of outcome. Ann Surg. 1998;227:566–71.
Ng JK, Urbanski SJ, Mangat N, et al. Colorectal liver metastases contact centripetally with a response to chemotherapy: a histomorphologic study. Cancer. 2008;112:362–71.
Kokudo N, Miki Y, Sugai S, et al. Genetic and histological assessment of surgical margins in resected liver metastases from colorectral carcinoma: minimum surgical margins for successful resection. Arch Surg. 2002;137:833–40.
Pawlik TM, Scoggins CR, Zorzi D, et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg. 2005;241:715–24.
Andreou A, Aloia T, Brouquet A, et al. Margin status remains an important determinant of survival after surgical resection of colorectal liver metastases in the era of modern chemotherapy. Ann Surg. 2013;257:1079–88.
Margonis GA, Spolverato G, Kim Y, et al. Intraoperative surgical margin re-resection for colorectal liver metastasis: is it worth the effort? J Gastrointest Surg. 2015;13:872–80.
Tranchart H, Chirica M, Faron M, et al. Prognostic impact of positive surgical margins after resection of colorectal cancer liver metastases: reappraisal in the era of modern chemotherapy. World J Surg. 2013;37:2647–54.
Adam R, Laurent A, Azoulay D, et al. Two-stage hepatectomy: a planned strategy to treat irresectable liver tumors. Ann Surg. 2000;232:777–85.
Schadde E, Ardiles V, Robles-Campos R, et al. Early survival and safety of ALPPS: first report of the international ALPPS registry. Ann Surg. 2014;260:829–38.
Adam R, de Hass RJ, Wicherts DA, et al. Concomitant extrahepatic disease in patients with colorectal liver metastases: when is there a place for surgery? Ann Surg. 2011;253:349–59.
Adam R, Pascal G, Castaing D, et al. Tumor progression while on chemotherapy: a contraindication to liver resection for multiple colorectal metastases? Ann Surg. 2004;240:1052–61.
Adam R, Delvart V, Pascal G, et al. Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy: a model to predict long-term survival. Ann Surg. 2004;240:644–57.
Adam R, Hoti E, Bredt LC, et al. Evolution of neoadjuvant therapy for extended hepatic metastases: have we reached our (non-resectable) limit? J Surg Oncol. 2010;102:922–31.
Adam R, de Gramont A, Figueras J, et al. The oncosurgery approach to managing liver metastases from colorectal cancer: a multidisciplinary international consensus. Oncologist. 2012;17:1225–39.
Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–16.
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Adam R, Wicherts DA, de Haas RJ, et al. Patients with initially unresectable colorectal liver metastases: is there a possibility of cure? J Clin Oncol. 2009;27:1829–35.
Goere D, Malka D, Tzanis D, et al. Is there a possibility of a cure in patients with colorectal peritoneal carcinomatosis amenable to complete cytoreductive surgery and intraperitoneal chemotherapy? Ann Surg. 2013;257:1065–71.
Sadot E, Koerkamp BG, Leal JN, et al. Resection margin and survival in 2368 patients undergoing hepatic resection for metastatic colorectal cancer: surgical technique of biologic surrogate? Ann Surg. 2015;262:476–85.
Hamady ZZ, Lodge JP, Welsh FK, et al. One-millimeter cancer-free margin is curative for colorectal liver metastases: a propensity score case-match approach. Ann Surg. 2014;259:543–8.
Viagnò L, Capussotti L, Barroso E, et al. Progression while receiving preoperative chemotherapy should not be an absolute contraindication to liver resection for colorectal metastases. Ann Surg Oncol. 2012;19:2786–96.
Tomlinson JS, Jarnagin WR, DeMatteo RP, et al. Actual 10-year survival after resection of colorectal liver metastases define cure. J Clin Oncol. 2007;25:4575–80.
Conflict of interest
All authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
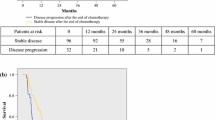
10434_2015_5060_MOESM2_ESM.tif
Difference between time to last unresectable recurrence and recurrence-free survival(RFS) of patients after R1 resection, demonstrating the effect of repeat surgery. Supplementary material 2 (TIFF 71 kb)
Rights and permissions
About this article
Cite this article
Hosokawa, I., Allard, MA., Gelli, M. et al. Long-Term Survival Benefit and Potential for Cure after R1 Resection for Colorectal Liver Metastases. Ann Surg Oncol 23, 1897–1905 (2016). https://doi.org/10.1245/s10434-015-5060-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-5060-8