Abstract
Background
No studies have examined the impact of the interval from conclusion of neoadjuvant chemotherapy to surgery in breast cancer patients. This study was undertaken to investigate the relationship between time interval from neoadjuvant chemotherapy to surgery and survival outcomes.
Methods
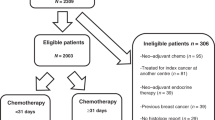
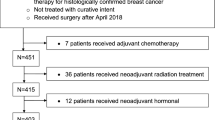
Breast cancer patients diagnosed with stage I–III disease who received neoadjuvant chemotherapy June 1995 to April 2007 were identified. The effect of neoadjuvant chemotherapy to surgery interval, defined as ≤4, 4–6, or >6 weeks, on survival outcomes was examined. Descriptive statistics and Cox proportional hazards models were used.
Results
A total of 1101 patients were identified. Median time to surgery was 33 (range 8–159) days; 335 patients (30.4 %) had surgery within 4 weeks of their last dose of neoadjuvant chemotherapy, 524 (47.6 %) within 4–6 weeks, and 242 (22.0 %) after more than 6 weeks. Median follow-up was 94 (range 3–178) months. The 5-year overall survival (OS) estimates were 79, 87, and 81 % in patients who underwent surgery ≤4, 4–6, and >6 weeks after neoadjuvant chemotherapy, respectively (p = 0.03). The three groups did not differ in 5-year recurrence-free survival (RFS) or locoregional recurrence-free survival (LRFS). In multivariable analysis, compared with an interval of ≤4 weeks, patients who underwent surgery at 4–6 or >6 weeks had equivalent OS, LRFS, and RFS; a sensitivity analysis suggested worse OS in patients who underwent surgery at >8 weeks.
Conclusions
Patients with neoadjuvant chemotherapy to surgery intervals of up to 8 weeks had equivalent OS, RFS, and LRFS.

Similar content being viewed by others
References
Mauri D, Pavlidis N, Ioannidis JPA. Neoadjuvant versus adjuvant systemic treatment in breast cancer: a meta-analysis. J Natl Cancer Inst. 2005;97(3):188–94.
Rastogi P, Anderson SJ, Bear HD, et al. Preoperative chemotherapy: updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J Clin Oncol. 2008;26(5):778–85.
Mittendorf EA, Buchholz TA, Tucker SL, et al. Impact of chemotherapy sequencing on local-regional failure risk in breast cancer patients undergoing breast-conserving therapy. Ann Surg. 2013;257(2):173–9.
Jara Sánchez C, Ruiz A, Martín M, et al. Influence of timing of initiation of adjuvant chemotherapy over survival in breast cancer: a negative outcome study by the Spanish Breast Cancer Research Group (GEICAM). Breast Cancer Res Treat. 2007;101(2):215–23.
Cold S, Düring M, Ewertz M, Knoop A, Møller S. Does timing of adjuvant chemotherapy influence the prognosis after early breast cancer? Results of the Danish Breast Cancer Cooperative Group (DBCG). Br J Cancer. 2005;93(6):627–32.
Shannon C, Ashley S, Smith IE. Does timing of adjuvant chemotherapy for early breast cancer influence survival? J Clin Oncol. 2003;21(20):3792–7.
Gagliato D, Gonzalez-Angulo AM, Lei X, et al. Clinical impact of delaying initiation of adjuvant chemotherapy in patients with breast cancer. J Clin Oncol. 2014;32(8):735–44.
Gunduz N, Fisher B, Saffer EA. Effect of surgical removal on the growth and kinetics of residual tumor. Cancer Res. 1979;39(10):3861–5.
Fisher B, Gunduz N, Coyle J, Rudock C, Saffer E. Presence of a growth-stimulating factor in serum following primary tumor removal in mice. Cancer Res. 1989;49(8):1996–2001.
Segatto I, Berton S, Sonego M, et al. Surgery-induced wound response promotes stem-like and tumor-initiating features of breast cancer cells, via STAT3 signaling. Oncotarget. 2014;5(15):6267–79.
Wolmark N, Wang J, Mamounas E, Bryant J, Fisher B. Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J Natl Cancer Inst Monogr. 2001;(30):96–102.
Bear HD, Anderson S, Brown A, et al. The effect on tumor response of adding sequential preoperative docetaxel to preoperative doxorubicin and cyclophosphamide: preliminary results from National Surgical Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol. 2003;21(22):4165–74.
Bear HD, Anderson S, Smith RE, et al. Sequential preoperative or postoperative docetaxel added to preoperative doxorubicin plus cyclophosphamide for operable breast cancer: National Surgical Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol. 2006;24(13): 2019–27.
Mauriac L, Durand M, Avril A, Dilhuydy JM. Effects of primary chemotherapy in conservative treatment of breast cancer patients with operable tumors larger than 3 cm. Results of a randomized trial in a single centre. Ann Oncol. 1991;2(5): 347–354.
Von Minckwitz G, Kümmel S, Vogel P, et al. Neoadjuvant vinorelbine-capecitabine versus docetaxel-doxorubicin-cyclophosphamide in early nonresponsive breast cancer: phase III randomized GeparTrio trial. J Natl Cancer Inst. 2008;100(8):542–51.
Gianni L, Pienkowski T, Im YH, et al. Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol. 2012;13(1):25–32.
Von Minckwitz G, Raab G, Caputo A, et al. Doxorubicin with cyclophosphamide followed by docetaxel every 21 days compared with doxorubicin and docetaxel every 14 days as preoperative treatment in operable breast cancer: the GEPARDUO study of the German Breast Group. J Clin Oncol. 2005;23(12):2676–85.
Makris A, Powles TJ, Ashley SE, et al. A reduction in the requirements for mastectomy in a randomized trial of neoadjuvant chemoendocrine therapy in primary breast cancer. Ann Oncol. 1998;9(11):1179–84.
Untch M, Rezai M, Loibl S, et al. Neoadjuvant treatment with trastuzumab in HER2-positive breast cancer: results from the GeparQuattro study. J Clin Oncol. 2010;28(12):2024–31.
Teoule P. Trojan J, Bechstein W, Woeste G. Impact of neoadjuvant chemotherapy on postoperative morbidity after gastrectomy for gastric cancer. Dig Surg. 2015;32(4):229–37.
Berkel AE, Woutersen DP, van der Palen J, Klaase JM. Prognostic factors for postoperative morbidity and tumour response after neoadjuvant chemoradiation followed by resection for rectal cancer. J Gastrointest Surg. 2014;18(9):1648–57.
Warren Peled A, Itakura K, Foster RD, et al. Impact of chemotherapy on postoperative complications after mastectomy and immediate breast reconstruction. Arch Surg. 2010;145(9):880–5.
Song J, Zhang X, Liu Q, et al. Impact of neoadjuvant chemotherapy on immediate breast reconstruction: a meta-analysis. PLoS One. 2014;9(5):e98225.
Disclosures
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sanford, R.A., Lei, X., Barcenas, C.H. et al. Impact of Time from Completion of Neoadjuvant Chemotherapy to Surgery on Survival Outcomes in Breast Cancer Patients. Ann Surg Oncol 23, 1515–1521 (2016). https://doi.org/10.1245/s10434-015-5020-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-5020-3