Abstract
Background
This study aimed to evaluate the role of surgery for patients with high-grade pancreatic neuroendocrine carcinoma (hgPNEC) in a large Nordic multicenter cohort study. Prior studies evaluating the role of surgery for patients with hgPNEC are limited, and the benefit of the surgery is uncertain.
Methods
Data from patients with a diagnosis of hgPNEC determined between 1998 and 2012 were retrospectively registered at 10 Nordic university hospitals. Kaplan–Meier curves were used to compare the overall survival of different treatment groups, and Cox-regression analysis was used to evaluate factors potentially influencing survival.
Results
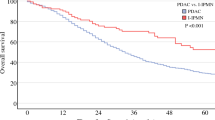
The study registered 119 patients. The median survival period from the time of metastasis was 23 months for patients undergoing initial resection of localized nonmetastatic disease and chemotherapy at the time of recurrence (n = 14), 29 months for patients undergoing resection of the primary tumor and resection/radiofrequency ablation of synchronous metastatic liver disease (n = 12), and 13 months for patients with synchronous metastatic disease given systemic chemotherapy alone (n = 78). The 3-year survival rate after surgery of the primary tumor and metastatic disease was 69 %. Resection of the primary tumor was an independent factor for improved survival after occurrence of metastatic disease.
Conclusions
Patients with resected localized nonmetastatic hgPNEC and later metastatic disease seemed to benefit from initial resection of the primary tumor. Patients selected for resection of the primary tumor and synchronous liver metastases had a high 3-year survival rate. Selected patients with both localized hgPNEC and metastatic hgPNEC should be considered for radical surgical treatment.


Similar content being viewed by others
References
Sorbye H, Welin S, Langer SW, et al. Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC study. Ann Oncol. 2013;24:152–60.
Cho MY, Kim JM, Sohn JH, et al. Current trends of the incidence and pathological diagnosis of gastroenteropancreatic neuroendocrine tumors (GEP-NETs) in Korea 2000–2009: multicenter Study. Cancer Res Treat. 2012;44:157–65.
Lepage C, Bouvier AM, Faivre J. Endocrine tumours: epidemiology of malignant digestive neuroendocrine tumours. Eur J Endocrinol. 2013;168:R77–83.
Bosman FT, Carneiro F, Hruban RH. WHO Classification of Tumours of the Digestive System. Lyon: International Agency for Research on Cancer (IARC), 2010.
Sorbye H, Strosberg J, Baudin E, Klimstra DS, Yao JC. Gastroenteropancreatic high-grade neuroendocrine carcinoma. Cancer. 2014;120:2814–23.
Panzuto F, Boninsegna L, Fazio N, et al. Metastatic and locally advanced pancreatic endocrine carcinomas: analysis of factors associated with disease progression. J Clin Oncol. 2011;29:2372–7.
Strosberg JR, Cheema A, Weber J, Han G, Coppola D, Kvols LK. Prognostic validity of a novel American Joint Committee on Cancer Staging Classification for pancreatic neuroendocrine tumors. J Clin Oncol. 2011;29:3044–9.
Basturk O, Tang L, Hruban RH, et al. Poorly differentiated neuroendocrine carcinomas of the pancreas: a clinicopathologic analysis of 44 cases. Am J Surg Pathol. 2014;38:437–47.
Fischer L, Bergmann F, Schimmack S, et al. Outcome of surgery for pancreatic neuroendocrine neoplasms. Br J Surg. 2014;101:1405–12.
Kinoshita K, Minami T, Ohmori Y, Kanayama S, Yoshikawa K, Tsujimura T. Curative resection of a small cell carcinoma of the pancreas: report of a case of long survival without chemotherapy. J Gastroenterol Hepatol. 2004;19:1087–91.
Winter JM, Narang AK, Mansfield AS, et al. Resectable pancreatic small cell carcinoma. Rare Tumors. 2011;3:e5.
Berkel S, Hummel F, Gaa J, et al. Poorly differentiated small cell carcinoma of the pancreas: a case report and review of the literature. Pancreatology. 2004;4:521–6.
Sorbye H, Westre B, Horn A. Curative surgery after neoadjuvant chemotherapy in metastatic poorly differentiated neuroendocrine carcinoma. Eur J Surg Oncol. 2007;33:1209–10.
Groeschl RT, Christians KK, Turaga KK, Gamblin TC. Management of primary hepatopancreatobiliary small cell carcinoma. J Surg Oncol. 2013;107:692–5.
Kolby L, Nilsson O, Ahlman H. Gastroduodenal endocrine tumours. Scand J Surg. 2004;93:317–23.
Akerstrom G. Management of carcinoid tumors of the stomach, duodenum, and pancreas. World J Surg. 1996;20:173–82.
Nilsson O, Van CE, Delle FG, et al. Poorly differentiated carcinomas of the foregut (gastric, duodenal, and pancreatic). Neuroendocrinology. 2006;84:212–5.
Strosberg JR, Coppola D, Klimstra DS, et al. The NANETS consensus guidelines for the diagnosis and management of poorly differentiated (high-grade) extrapulmonary neuroendocrine carcinomas. Pancreas. 2010;39:799–800.
Kunz PL, Reidy-Lagunes D, Anthony LB, et al. Consensus guidelines for the management and treatment of neuroendocrine tumors. Pancreas. 2013;42:557–77.
Oberg K, Knigge U, Kwekkeboom D, Perren A. Neuroendocrine gastro-entero-pancreatic tumors: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23(Suppl 7):vii124–30.
Rindi G, Kloppel G, Alhman H, et al. TNM staging of foregut (neuro)endocrine tumors: a consensus proposal including a grading system. Virchows Arch. 2006;449:395–401.
Hadoux J, Malka D, Planchard D, et al. Post-first-line FOLFOX chemotherapy for grade 3 neuroendocrine carcinoma. Endocr Relat Cancer. 2015;22:289–98.
Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–55.
StataCorp. Stata Statistical Software: Release 13. College Station: StataCorp LP, 2013.
Winter JM, Brennan MF, Tang LH, et al. Survival after resection of pancreatic adenocarcinoma: results from a single institution over three decades. Ann Surg Oncol. 2012;19:169–75.
Smith JD, Reidy DL, Goodman KA, Shia J, Nash GM. A retrospective review of 126 high-grade neuroendocrine carcinomas of the colon and rectum. Ann Surg Oncol. 2014;21:2956–62.
Korse CM, Taal BG, van Velthuysen ML, Visser O. Incidence and survival of neuroendocrine tumours in the Netherlands according to histological grade: experience of two decades of cancer registry. Eur J Cancer. 2013;49:1975–83.
Yang Z, Tang LH, Klimstra DS. Gastroenteropancreatic neuroendocrine neoplasms: historical context and current issues. Semin Diagn Pathol. 2013;30:186–96.
Velayoudom-Cephise FL, Duvillard P, Foucan L, et al. Are G3 ENETS neuroendocrine neoplasms heterogeneous? Endocr Relat Cancer. 2013;20:649–57.
Basturk O, Yang Z, Tang LH. Increased (>20%) KI67 proliferation index in morphologically well-differentiated pancreatic neuroendocrine tumors (pannets) correlates with decreased overall survival. Lab Invest. 2013;93(Suppl 1):4234.
Shi C, Gonzalez RS, Zhao Z, et al. Liver metastases of small intestine neuroendocrine tumors: Ki-67 heterogeneity and World Health Organization grade discordance with primary tumors. Am J Clin Pathol. 2015;143:398–404.
Zen Y, Heaton N. Elevated Ki-67 labeling index in “synchronous liver metastases” of well-differentiated enteropancreatic neuroendocrine tumor. Pathol Int. 2013;63:532–8.
Acknowledgment
The study was initiated by the Nordic Neuroendocrine Tumor Group. We thank Randi Eikeland (Clinical Cancer Research Office, Haukeland University Hospital, Bergen, Norway) for assisting with data management. The study was supported by grants from the Nordic Cancer Union and Eckbo Foundations. Halfdan Sorbye received funding from the Norwegian Cancer Society; Eva Tiensuu Janson received a research grant from the Swedish Cancer Society; and Henning Grønbæk received a clinical research grant from the Novo Nordisk Foundation.
Disclosure
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haugvik, SP., Janson, E.T., Österlund, P. et al. Surgical Treatment as a Principle for Patients with High-Grade Pancreatic Neuroendocrine Carcinoma: A Nordic Multicenter Comparative Study. Ann Surg Oncol 23, 1721–1728 (2016). https://doi.org/10.1245/s10434-015-5013-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-5013-2