Abstract
Background
The TNM classification for distal cholangiocarcinoma was first introduced in the 7th edition, which was published in 2009; however, prognostic accuracy compared with the 5th and 6th editions has not yet been evaluated and requires validation.
Methods
A prospective histological database of patients with distal bile duct cancer was analyzed, and histological parameters and stage of the distal cholangiocarcinoma were assessed according to the 5th, 6th, and 7th editions of the TNM classification.
Results
Between 1994 and 2012, a total of 516 patients underwent pancreatic head resection, of whom 59 patients (11.4 %) experienced histologically confirmed distal cholangiocarcinoma. The median overall survival time was 22.2 months (13.1–31.4). Tumor recurrence occurred in 23 patients after a median disease-free survival time of 14.1 months. The 7th edition showed a monotonicity of all gradients, with a stepwise increase of mortality related to a stepwise increase of tumor stage (log-rank test; p < 0.05) demonstrating best discrimination of all tested editions [area under the receiver operating characteristic curve (AUC) 0.82; 95 % CI 0.70–0.95; p = 0.012]. The discrimination rate was low for the 5th (AUC 0.67; 95 % CI 0.42–0.91; p = 0.18) and 6th editions (AUC 0.70; 95 % CI 0.47–0.93; p = 0.11), while the log-rank test did not reach statistical significance. On multivariate analysis, lymph node involvement and positive resection margins were positive and independent predictors of inferior survival (p < 0.05).
Conclusions
The 7th edition of the TNM classification was favorable in terms of predicting outcome, and generated a monotonicity of all grades. Strikingly, the 7th edition, but not the 5th and 6th editions, was of prognostic significance to predict outcome.
Similar content being viewed by others
References
Beahrs OH, Henson DE, Hutter RVP, et al. Manual for staging of cancer. 3rd ed. Philadelphia: Lippincott; 1988.
Beahrs OH, Henson DE, Hutter RVP, et al. Manual for staging of cancer. 4th ed. Philadelphia (PA): Lippincott; 1992.
Fleming ID, Cooper JS, Henson DE, et al. AJCC cancer staging manual. 5th ed. Philadelphia: Lippincott-Raven; 1997.
Greene FL, Page DL, Fleming ID, et al. AJCC cancer staging manual. 6th ed. New York: Springer; 2002.
Sobin LH, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours. 7th ed. Chichester: Wiley; 2009.
Nakeeb A, Pitt HA, Sohn TA, et al. Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors. Ann Surg. 1996;224(4):463–73; discussion 473–5.
Cardinale V, Semeraro R, Torrice A, et al. Intra-hepatic and extra-hepatic cholangiocarcinoma: new insight into epidemiology and risk factors. World J Gastrointest Oncol. 2010;2(11):407–16.
Jepsen P, Vilstrup H, Tarone RE, Friis S, Sørensen HT. Incidence rates of intra- and extrahepatic cholangiocarcinomas in Denmark from 1978 through 2002. J Natl Cancer Inst. 2007;99(11):895–7.
Chung YJ, Choi DW, Choi SH, Heo JS, Kim DH. Prognostic factors following surgical resection of distal bile duct cancer. J Korean Surg Soc. 2013;85(5):212–8.
Shaib Y, El-Serag HB. The epidemiology of cholangiocarcinoma. Semin Liver Dis. 2004;24(2):115–5.
Tol JA, Gouma DJ, Bassi C, et al.; International Study Group on Pancreatic Surgery. Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: a consensus statement by the International Study Group on Pancreatic Surgery (ISGPS). Surgery. 2014;156(3):591–600.
Hong S, Kim M, Pi DY, et al. Analysis of extrahepatic bile duct carcinomas according to the New American Joint Committee on Cancer staging system focused on tumor classification problems in 222 patients. Cancer. 2005;104(4):802–10.
Tan X, Xiao K, Liu W, Chang S, Zhang T, Tang H. Prognostic factors of distal cholangiocarcinoma after curative surgery: a series of 84 cases. Hepatogastroenterology. 2013;60(128):1892–5.
DeOliveira ML, Cunningham SC, Cameron JL, et al. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg. 2007;245(5):755–2.
Cheng Q, Luo X, Zhang B, Jiang X, Yi B, Wu M. Distal bile duct carcinoma: prognostic factors after curative surgery. A series of 112 cases. Ann Surg Oncol. 2007;14(3):1212–9.
Wittekind C, Compton CC, Greene FL, Sobin LH. TNM residual tumor classification revisited. Cancer. 2002;94(9):2511–6.
Ebata T, Nagino M, Nishio H, Igami T, Yokoyama Y, Nimura Y. Pancreatic and duodenal invasion in distal bile duct cancer: paradox in the tumor classification of the American Joint Committee on Cancer. World J Surg. 2007;31(10):2008–2015.
Kim HJ, Kim CY, Hur YH, et al. The prognostic factors for survival after curative resection of distal cholangiocarcinoma: perineural invasion and lymphovascular invasion. Surg Today. 2014;44(10):1879–86.
Bahra M, Jacob D, Langrehr JM, Neumann UP, Neuhaus P. Carcinoma of the distal and middle bile duct: surgical results, prognostic factors, and long-term follow-up. J Hepatobiliary Pancreat Surg. 2008;15(5):501–7.
Choi SB, Park SW, Kim KS, Choi JS, Lee WJ. The survival outcome and prognostic factors for middle and distal bile duct cancer following surgical resection. J Surg Oncol. 2009;99(6):335–42.
Tan X, Xiao K, Liu W, Chang S, Zhang T, Tang H. Distal cholangiocarcinoma: prognostic factors after curative surgery. A series of 84 cases. Hepatogastroenterology. 2013;60(128):1892–5.
Murakami Y, Uemura K, Sudo T, et al. Prognostic factors after surgical resection for intrahepatic, hilar, and distal cholangiocarcinoma. Ann Surg Oncol. 2011;18(3):651–8.
Altman DG, Bland JM. Absence of evidence is not evidence of absence. BMJ. 1995;311(7003):485.
Acknowledgment
Felix Krenzien was supported by the German Research Foundation (KR 4362/2-1). None of the authors have received any financial benefit.
Conflicts of interest
Georg Wiltberger, Felix Krenzien, Christian Benzing, Georgi Atanasov, Fritz Klein, Hans-Michael Hau, Linda Feldbrügge, Johann Pratschke, Moritz Schmelzle, and Sven Jonas declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Georg Wiltberger and Felix Krenzien contributed equally to this work and are co-first authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10434_2015_4999_MOESM1_ESM.tif
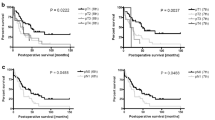
Survival curves according different pathological characteristics. The absence of residual Tumor (A), the absence of lymph node metastasis (B), a well/moderately differentiated tumor (C) showed survival benefit for patients who underwent partial pancreaticoduodenectomy (p<0.05). Log Rank test was used to compare survival curves.Survival curves according different pathological characteristics. The absence of residual Tumor (A), the absence of lymph node metastasis (B), a well/moderately differentiated tumor (C) showed survival benefit for patients who underwent partial pancreaticoduodenectomy (p<0.05). Log Rank test was used to compare survival curves. (TIFF 1233 kb)
10434_2015_4999_MOESM2_ESM.tif
Survival curves according different pathological characteristics. Invasion of small lymphatic vessels (A), vessel invasion (B), perineural invasion (C), distant metastasis (D), pancreas infiltration (E) and duodenal infiltration (F) did not statistically affect patient outcome. Log Rank test was used to compare survival curves. (TIFF 1662 kb)
Rights and permissions
About this article
Cite this article
Wiltberger, G., Krenzien, F., Benzing, C. et al. Prognostic Accuracy of the Seventh Edition of the TNM Classification Compared with the Fifth and Sixth Edition for Distal Cholangiocarcinoma. Ann Surg Oncol 23, 1320–1326 (2016). https://doi.org/10.1245/s10434-015-4999-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4999-9