Abstract
Background
Previous reports on the outcome of surgery for colorectal cancer lung metastases (CRCLM) have come from high-volume centers. This report describes the outcomes achieved in the general population of Ontario.
Methods
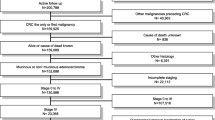
All patients in Ontario who underwent resection of CRCLM between 1994 and 2009 were identified using the population-based Ontario Cancer Registry. Electronic treatment records identified surgical procedures and chemotherapy delivery. This report describes the volume of resections for CRCLM in relation to the incidence of colorectal cancer (CRC). Temporal trends in practice are described during three periods: 1994–1999, 2000–2004, and 2005–2009. Overall survival (OS) and cancer-specific survival (CSS) were measured from the time of lung resection.
Results
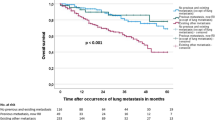
A total of 709 patients underwent resection of CRCLM. Between 1994 and 2009, surgical volume increased 190 %, from 1 resection for every 282 incident cases to 1 resection for every 97 incident cases (p < 0.001). The use surgery for CRCLM varied considerably between regions, from 1 resection per 95 incident cases to 1 resection per 212 incident cases (p = 0.021). Use of perioperative chemotherapy increased during study periods, from 22 % (28/130) to 34 % (73/217) to 40 % (146/362; p < 0.001). Utilization rates varied across geographic regions (range 21–59 %; p = 0.005). The OS rate was 40 % [95 % confidence interval (CI) 36–44 %] at 5 years and 27 % (95 % CI 23–31 %) at 10 years. The CSS rate was 42 % (95 % CI 38–46 %) at 5 years and 32 % (95 % CI 27–37 %) at 10 years.
Conclusions
A proportion of patients with resected CRCLM will achieve long-term survival. Outcomes in routine practice are comparable with those reported for high-volume centers. The use of surgery varies considerably across Ontario.



Similar content being viewed by others
References
Pfannschmidt J, Dienemann H, Hoffmann H. Surgical resection of pulmonary metastases from colorectal cancer: a systematic review of published series. Ann Thorac Surg. 2007;84:324–38.
Iida T, Nomori H, Shiba M, et al. Prognostic factors after pulmonary metastasectomy for colorectal cancer and rationale for determining surgical indications: a retrospective analysis. Ann Surg. 2013;257:1059–64.
Salah S, Watanabe K, Welter S, et al. Colorectal cancer pulmonary oligometastases: pooled analysis and construction of a clinical lung metastasectomy prognostic model. Ann Oncol. 2012;23:2649–55.
Peppercorn JM, Weeks JC, Cook EF, et al. Comparison of outcomes in cancer patients treated within and outside clinical trials: conceptual framework and structured review. Lancet. 2004;363:263–70.
Templeton AJ, Vera-Badillo FE, Wang L, et al. Translating clinical trials to clinical practice: outcomes of men with metastatic castration resistant prostate cancer treated with docetaxel and prednisone in and out of clinical trials. Ann Oncol. 2013;24:2972–7.
Booth CM, Siemens DR, Li G, et al. Perioperative chemotherapy for muscle-invasive bladder cancer: a population-based outcomes study. Cancer. 2014;120:1630–8.
Meyer RM. Generalizing the results of cancer clinical trials. J Clin Oncol. 2010;28:187–9.
Booth CM, Mackillop WJ. Translating new medical therapies into societal benefit: the role of population-based outcome studies. JAMA. 2008;300:2177–9.
Booth CM, Tannock IF. Randomised controlled trials and population-based observational research: partners in the evolution of medical evidence. Br J Cancer. 2014;110:551–5.
Clarke EA, Marrett LD, Krieger N. Cancer registration in Ontario: a computer approach. In: Jenson OM, Parkin DM, MacLennan R, editors. Cancer registration principles and methods. Lyon: IARC; 1991. p. 246–57.
Williams J, Young W. A summary of studies on the quality of health care administrative databases in Canada. In: Goel V, Williams JI, Anderson GM, et al, editors. Patterns of health care in Ontario: The ICES practice atlas. 2nd ed. Ottawa: Canadian Medical Association; 1996. p. 339–45.
Mackillop WJ, Zhang-Salomons J, Groome PA, et al. Socioeconomic status and cancer survival in Ontario. J Clin Oncol. 1997;15:1680–9.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9.
Booth CM, Li G, Biagi JJ, et al. Surgical resection and perioperative chemotherapy for colorectal cancer (CRC) liver metastases in routine clinical practice: a population-based outcomes study. Eur J Surg Oncol. 2015. doi:10.1016/j.ejso.2015.10.006.
Nordlinger B, Sorbye H, Glimelius B, et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet. 2008;371:1007–16.
Sundaresan S, McLeod R, Irish J, et al. Early results after regionalization of thoracic surgical practice in a single-payer system. Ann Thorac Surg. 2013;95:472–8.
Acknowledgment
The authors gratefully acknowledge the contributions of Dr. Ryan Fitzpatrick, Janine Biagi and Tina Dyer in the performance of this study. Parts of this material are based on data and information provided by Cancer Care Ontario. However, the analysis, conclusions, opinions, and statements expressed herein are those of the authors and not necessarily those of Cancer Care Ontario. This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results, and conclusions reported in this article are those of the authors and independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Dr. Booth had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Booth is supported as a Canada Research Chair in Population Cancer Care. This work also was supported by the Canada Foundation for Innovation and Queen’s University Department of Oncology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Booth, C.M., Nanji, S., Wei, X. et al. Outcomes of Resected Colorectal Cancer Lung Metastases in Routine Clinical Practice: A Population-Based Study. Ann Surg Oncol 23, 1057–1063 (2016). https://doi.org/10.1245/s10434-015-4979-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4979-0