Abstract
Background
This study aimed to compare the utility of the number of positive lymph nodes with the lymph node ratio (LNR) in predicting survival after resection of extrahepatic cholangiocarcinoma.
Methods
A retrospective analysis of 142 consecutive patients who underwent radical resection of extrahepatic cholangiocarcinoma was performed. A total of 3066 regional lymph nodes were resected. The median number of nodes per patient was 21. The optimal cutoff values for the number of positive nodes and the LNR were determined using the Chi square scores calculated by the Cox proportional hazards regression model.
Results
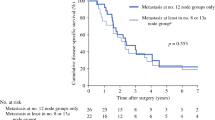
Nodal disease was found in 59 patients (42 %). In the subsequent analysis of the impact that nodal status has on survival, 18 patients with R1/2 resection and 6 patients with paraaortic nodal disease who did not survive for more than 5 years after resection were excluded. The optimal cutoff value for the number of positive nodes was 1, and the optimal cutoff value for the LNR was 5 %. Univariate analysis identified both the number of positive nodes (0, 1, or ≥2; P = 0.005) and the LNR (0, 0–5, or >5 %; P = 0.007) as significant prognostic factors. Multivariate analysis identified the number of positive nodes but not the LNR as an independent prognostic factor (P = 0.012). The 5-year survival rates were 64 % for the patients with no positive nodes, 46 % for the patients with one positive node, and 28 % for the patients with two or more positive nodes.
Conclusions
The number of positive lymph nodes predicts survival better than the LNR after resection of extrahepatic cholangiocarcinoma, provided that nodal evaluation is sufficient.

Similar content being viewed by others
References
Wang J, Dang P, Raut CP, et al. Comparison of a lymph node ratio-based staging system with the 7th AJCC system for gastric cancer: analysis of 18,043 patients from the SEER database. Ann Surg. 2012;255:478–85.
Mariette C, Piessen G, Briez N, Triboulet JP. The number of metastatic lymph nodes and the ratio between metastatic and examined lymph nodes are independent prognostic factors in esophageal cancer regardless of neoadjuvant chemoradiation or lymphadenectomy extent. Ann Surg. 2008;247:365–71.
Rosenberg R, Engel J, Bruns C, et al. The prognostic value of lymph node ratio in a population-based collective of colorectal cancer patients. Ann Surg. 2010;251:1070–8.
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A III (eds). AJCC cancer staging manual. 7th ed. New York: Springer; 2010.
Bhatti I, Peacock O, Awan AK, Semeraro D, Larvin M, Hall RI. Lymph node ratio versus number of affected lymph nodes as predictors of survival for resected pancreatic adenocarcinoma. World J Surg. 2010;34:768–75.
Riediger H, Keck T, Wellner U, zur Hausen A, Adam U, Hopt UT, et al. The lymph node ratio is the strongest prognostic factor after resection of pancreatic cancer. J Gastrointest Surg. 2009;13:1337–44.
Negi SS, Singh A, Chaudhary A. Lymph nodal involvement as prognostic factor in gallbladder cancer: location, count or ratio? J Gastrointest Surg. 2011;15:1017–25.
Murakami Y, Uemura K, Sudo T, et al. Number of metastatic lymph nodes, but not lymph node ratio, is an independent prognostic factor after resection of pancreatic carcinoma. J Am Coll Surg. 2010;211:196–204.
Sierzega M, Nowak K, Kulig J, Matyja A, Nowak W, Popiela T. Lymph node involvement in ampullary cancer: the importance of the number, ratio, and location of metastatic nodes. J Surg Oncol. 2009;100:19–24.
Sakata J, Shirai Y, Wakai T, Ajioka Y, Akazawa K, Hatakeyama K. Assessment of the nodal status in ampullary carcinoma: the number of positive lymph nodes versus the lymph node ratio. World J Surg. 2011;35:2118–24.
Shirai Y, Sakata J, Wakai T, Ohashi T, Ajioka Y, Hatakeyama K. Assessment of lymph node status in gallbladder cancer: location, number, or ratio of positive nodes. World J Surg Oncol. 2012;10:87.
Kawai M, Tani M, Kobayashi Y, et al. The ratio between metastatic and examined lymph nodes is an independent prognostic factor for patients with resectable middle and distal bile duct carcinoma. Am J Surg. 2010;199:447–52.
Guglielmi A, Ruzzenente A, Campagnaro T, et al. Prognostic significance of lymph node ratio after resection of peri-hilar cholangiocarcinoma. HPB. 2011;13:240–5.
Sasaki R, Takahashi M, Funato O, et al. Prognostic significance of lymph node involvement in middle and distal bile duct cancer. Surgery. 2001;129:677–83.
Yoshida T, Matsumoto T, Sasaki A, Morii Y, Aramaki M, Kitano S. Prognostic factors after pancreatoduodenectomy with extended lymphadenectomy for distal bile duct cancer. Arch Surg. 2002;137:69–73.
Hong SM, Cho H, Lee OJ, Ro JY. The number of metastatic lymph nodes in extrahepatic bile duct carcinoma as a prognostic factor. Am J Surg Pathol. 2005;29:1177–83.
Murakami Y, Uemura K, Hayashidani Y, Sudo T, Ohge H, Sueda T. Pancreatoduodenectomy for distal cholangiocarcinoma: prognostic impact of lymph node metastasis. World J Surg. 2007;31:337–42.
Aoba T, Ebata T, Yokoyama Y, et al. Assessment of nodal status for perihilar cholangiocarcinoma: location, number, or ratio of involved nodes. Ann Surg. 2013;257:718–25.
Kiriyama M, Ebata T, Aoba T, Kaneoka Y, Arai T, Shimizu Y, et al. Prognostic impact of lymph node metastasis in distal cholangiocarcinoma. Br J Surg. 2015;102:399–406.
Shirai Y, Wakai T, Sakata J, Hatakeyama K. Regional lymphadenectomy for gallbladder cancer: rational extent, technical details, and patient outcomes. World J Gastroenterol. 2012;18:2775–83.
Shirai Y, Wakai T, Hatakeyama K. Radical lymph node dissection for gallbladder cancer: indications and limitations. Surg Oncol Clin N Am. 2007;16:221–32.
Greene FL, Page DL, Fleming ID, Fritz AG, Balch CM, Haller DG, et al. (eds). AJCC cancer staging manual. 6th ed. New York: Springer; 2002.
DeOliveira ML, Cunningham SC, Cameron JL, et al. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg. 2007;245:755–62.
Wakai T, Shirai Y, Moroda T, Yokoyama N, Hatakeyama K. Impact of ductal resection margin status on long-term survival in patients undergoing resection for extrahepatic cholangiocarcinoma. Cancer. 2005;103:1210–6.
Igami T, Nagino M, Oda K, Nishio H, Ebata T, Yokoyama Y, et al. Clinicopathologic study of cholangiocarcinoma with superficial spread. Ann Surg. 2009;249:296–302.
Peyre CG, Hagen JA, DeMeester SR, et al. The number of lymph nodes removed predicts survival in esophageal cancer: an international study on the impact of extent of surgical resection. Ann Surg. 2008;248:549–56.
Konstadoulakis MM, Roayaie S, Gomatos IP, Labow D, Fiel MI, Miller CM, et al. Aggressive surgical resection for hilar cholangiocarcinoma: is it justified? Audit of a single center’s experience. Am J Surg. 2008;196:160–9.
Juntermanns B, Sotiropoulos GC, Radunz S, et al. Comparison of the sixth and the seventh editions of the UICC classification for perihilar cholangiocarcinoma. Ann Surg Oncol. 2013;20:277–84.
Ito K, Ito H, Allen PJ, et al. Adequate lymph node assessment for extrahepatic bile duct adenocarcinoma. Ann Surg. 2010;251:675–81.
Chang GJ, Rodriguez-Bigas MA, Skibber JM, Moyer VA. Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst. 2007;99:433–41.
Son T, Hyung WJ, Lee JH, et al. Clinical implication of an insufficient number of examined lymph nodes after curative resection for gastric cancer. Cancer. 2012;118:4687–93.
Schwarz RE, Smith DD. Lymph node dissection impact on staging and survival of extrahepatic cholangiocarcinomas, based on U.S. population data. J Gastrointest Surg. 2007;11:158–65.
Kitagawa Y, Nagino M, Kamiya J, et al. Lymph node metastasis from hilar cholangiocarcinoma: audit of 110 patients who underwent regional and paraaortic node dissection. Ann Surg. 2001;233:385–92.
Neuhaus P, Jonas S, Bechstein WO, et al. Extended resections for hilar cholangiocarcinoma. Ann Surg. 1999;230:808–18.
Capussotti L, Muratore A, Polastri R, Ferrero A, Massucco P. Liver resection for hilar cholangiocarcinoma: in-hospital mortality and long-term survival. J Am Coll Surg. 2002;195:641–7.
Conflict of interest
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sakata, J., Wakai, T., Matsuda, Y. et al. Comparison of Number Versus Ratio of Positive Lymph Nodes in the Assessment of Lymph Node Status in Extrahepatic Cholangiocarcinoma. Ann Surg Oncol 23, 225–234 (2016). https://doi.org/10.1245/s10434-015-4609-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4609-x