Abstract
Background
With the rising cost of healthcare delivery and bundled payments for episodes of care, there has been impetus to minimize hospitalization and increase utilization of outpatient surgery mechanisms. Given the increase in outpatient mastectomy and immediate tissue expander (TE)-based reconstruction and the paucity of data on its comparative safety to inpatient procedures, we sought to understand the risk for early postoperative complications in an outpatient model compared with more traditional inpatient status using the National Surgical Quality Improvement Program database.
Methods
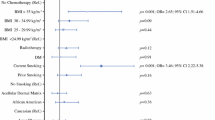
NSQIP data files from 2005 to 2012 were queried to identify patients undergoing immediate TE-based breast reconstruction after mastectomy. Patients were stratified by whether they received outpatient or inpatient care and then propensity score matched based on preoperative baseline characteristics to produce matched cohorts. Multivariate regression analysis was used to determine whether outpatient versus inpatient status conferred differing risk for 30-days complications.
Results
Of the 2014 patients who met criteria, 1:1 propensity matching yielded 634 patients in each of the matched cohorts. Overall complications (5.2 vs. 5.4 %), overall surgical complications (4.3 vs. 3.9 %), overall medical complications (1.3 vs. 2.1 %), and return to the operating room (6.6 vs. 7.3 %) were similar between outpatient and inpatients cohorts (p > .2), respectively. There was a small, but significant increased risk of organ/space SSI in outpatients (1.9 vs. 0.5 %, p = .02) and trend for increased risk for pulmonary embolus (PE) and urinary tract infection (UTI) in inpatients (0.3 vs. 0 %, p = .16; 0.3 vs. 0 %, p = .16).
Conclusions
Our studies suggest that outpatient TE confers similar safety profiles to inpatient TE with regards to 30-day postoperative overall complications, medical and surgical morbidity, and return to the operating room. A slightly increased risk for surgical site infection must be balanced against potential risk for known inpatient-related complications such as UTI and PE.
Similar content being viewed by others
References
Warren JL, Riley GF, Potosky AL, Klabunde CN, Richter E, Ballard-Barbash R. Trends and outcomes of outpatient mastectomy in elderly women. J Natl Cancer Inst. 1998;90:833–40.
Case C, Johantgen M, Steiner C. Outpatient mastectomy: clinical, payer, and geographic influences. Health Serv Res. 2001;36:869–84.
Ferrante, J, Gonzalez E, Pal N, Roetzheim R. The use and outcomes of outpatient mastectomy in Florida. Am J Surg. 2000;179:253–9; discussion 259–60.
Kruper L, Xu XX, Henderson K, Bernstein L, Chen SL. Utilization of mastectomy and reconstruction in the outpatient setting. Ann Surg Oncol. 2013;20:828–35.
Bian J, Krontiras H, Allison H. Outpatient mastectomy and breast reconstructive surgery. Ann Surg Oncol. 2008;15:1032–9.
Simpson SA, Ying BL, Ross LA, et al. Incidence of complications in outpatient mastectomy with immediate reconstruction. J Am Coll Surg. 2007;205:463–7.
Xue DQ, Qian C, Yang L, Wang XF., Risk factors for surgical site infections after breast surgery: a systematic review and meta-analysis. Eur J Surg Oncol. 2012;38:375–81.
Shaikh-Naidu N, Preminger BA, Rogers K, Messina P, Gayle LB. Determinants of aesthetic satisfaction following TRAM and implant breast reconstruction. Ann Plast Surg. 2004;52:465–70; discussion 470.
Gurunluoglu R, Gurunluoglu A, Williams SA, Tebockhorst S. Current trends in breast reconstruction: survey of American Society of Plastic Surgeons 2010. Ann Plast Surg. 2013;70:103–10.
Cema, Y, Albornoz CR, Disa JJ, et al. A paradigm shift in U.S. breast reconstruction: Part 2. The influence of changing mastectomy patterns on reconstructive rate and method. Plast Reconstr Surg. 2013;131:320e–6e.
Albornoz CR, Albornoz CR, Disa JJ, et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131:15–23.
Fischer JP, Nelson JA, Serletti JM, Wu LC. Peri-operative risk factors associated with early tissue expander (TE) loss following immediate breast reconstruction (IBR): a review of 9305 patients from the 2005-2010 ACS-NSQIP datasets. J Plast Reconstr Aesthet Surg. 2013;66:1504–12.
Fischer JP, Wes AM, Tuggle CT 3rd, Serletti JM, Wu LC. Risk analysis of early implant loss after immediate breast reconstruction: a review of 14,585 patients. J Am Coll Surg. 2013;217:983–90.
Peled AW, Stover AC, Foster RD, McGrath MH, Hwang ES. Long-term reconstructive outcomes after expander-implant breast reconstruction with serious infectious or wound-healing complications. Ann Plast Surg. 2012;68:369–73.
Birkmeyer JD, Shahian DM, Dimick JB, et al. Blueprint for a new American College of Surgeons: National Surgical Quality Improvement Program. J Am Coll Surg. 2008;207:777–82.
Ingraham AM, Richards KE, Hall BL, Ko CY. Quality improvement in surgery: the American College of Surgeons National Surgical Quality Improvement Program approach. Adv Surg. 2010;44:251–67.
Austin PC. Some methods of propensity-score matching had superior performance to others: results of an empirical investigation and Monte Carlo simulations. Biom J. 2009;51:171–84.
Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10:150–61.
Austin PC. A comparison of 12 algorithms for matching on the propensity score. Stat Med. 2014;33:1057–69.
Merkow RP, Bilimoria KY, Hall BL. Interpretation of the C-statistic in the context of ACS-NSQIP models. Ann Surg Oncol. 2011;18 Suppl 3:S295; author reply S296.
Paul P, Pennell ML, Lemeshow S. Standardizing the power of the Hosmer-Lemeshow goodness of fit test in large data sets. Stat Med. 2013;32:67–80.
Washer LL, Gutowski K. Breast implant infections. Infect Dis Clin North Am. 2012;26:111–25.
Khavanin N, Mlodinow A, Kim JY, Ver Halen JP, Antony AK, Samant S. Assessing safety and outcomes in outpatient versus inpatient thyroidectomy using the NSQIP: a propensity score matched analysis of 16,370 patients. Ann Surg Oncol. 2015;22:429–36.
Clayton JL, Bazakas A, Lee CN, Hultman CS, Halvorson EG. Once is not enough: withholding postoperative prophylactic antibiotics in prosthetic breast reconstruction is associated with an increased risk of infection. Plast Reconstr Surg. 2012;130:495–502.
Lu L, Fine NA. The efficacy of continuous local anesthetic infiltration in breast surgery: reduction mammaplasty and reconstruction. Plast Reconstr Surg. 2005;115:1927–34; discussion 1935–6.
Pacik PT, Nelson CE, Werner C. Pain control in augmentation mammaplasty: safety and efficacy of indwelling catheters in 644 consecutive patients. Aesthet Surg J. 2008;28:279–84.
Ethical Approval
De-identified patient information is freely available to all institutional members who comply with the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) Data Use Agreement. The Data Use Agreement implements the protections afforded by the Health Insurance Portability and Accountability Act of 1996 and the ACS-NSQIP Hospital Participation Agreement and conforms to the Declaration of Helsinki.
Disclaimer
The NSQIP and the hospitals participating in the NSQIP are the source of the data used herein; they have not been verified and are not responsible for the statistical validity of the data analysis, or the conclusions derived by the authors of this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Charles Qin and Anuja K Antony are co-first authors.
Rights and permissions
About this article
Cite this article
Qin, C., Antony, A.K., Aggarwal, A. et al. Assessing Outcomes and Safety of Inpatient Versus Outpatient Tissue Expander Immediate Breast Reconstruction. Ann Surg Oncol 22, 3724–3729 (2015). https://doi.org/10.1245/s10434-015-4407-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4407-5