Abstract
Purpose
Morphological subtypes of intraductal papillary mucinous neoplasm (IPMN) have been established. Invasive IPMNs include colloid carcinoma and tubular carcinoma. Few studies have explored the association between the morphological and invasive subtypes in a large population. Clinical relevance of the morphological subtypes remains unclear.
Methods
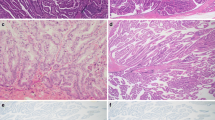
One hundred sixty-nine consecutive patients who underwent curative resection of IPMN were enrolled. The intraductal components were classified into four distinct epithelial subtypes: gastric, intestinal, pancreatobiliary, and oncocytic. The invasive components were classified as colloid or tubular.
Results
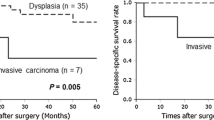
The numbers of patients with gastric, intestinal, pancreatobiliary, and oncocytic subtypes were 123, 42, 3, and 1, respectively. Fifty-six patients had invasive cancer (tubular type, 42; colloid type, 14). The proportions of gastric type IPMN within each histological grade were 88 % among adenomas, 43 % among noninvasive carcinomas, 41 % among minimally invasive carcinomas, and 74 % among invasive carcinomas. Gastric subtype was more commonly associated with branch duct type and intestinal subtype with main duct type, and these tendencies were statistically significant (P = 0.0131). Furthermore, there was a strong correlation between gastric and tubular types and between intestinal and colloid types (P < 0.0001). The 5-year survival rate among the 56 invasive cancers was 52.7 % for gastric type and 89.7 % for intestinal type, which was statistically significant (P = 0.030).
Conclusions
Gastric type IPMN is mostly derived from branch duct IPMN and often demonstrates benign behavior, as seen with adenomas. However, once gastric type IPMN develops into invasive carcinoma, the survival rate is significantly lower than other types.



Similar content being viewed by others
References
Furukawa T, Takahashi T, Kobari M, Matsuno S. The mucus-hypersecreting tumor of the pancreas. Development and extension visualized by three-dimensional computerized mapping. Cancer. 1992;70:1505–13.
Hruban RH, Pitman M, Klimstra DS. Tumors of the Pancreas. Washington, DC: American Registry of Pathology; 2007.
Furukawa T, Kloppel G, Volkan Adsay N, Albores-Saavedra J, Fukushima N, Horii A, et al. Classification of types of intraductal papillary-mucinous neoplasm of the pancreas: a consensus study. Virchows Arch. 2005;447:794–9.
Farrell JJ, Brugge WR. Intraductal papillary mucinous tumor of the pancreas. Gastrointest Endosc. 2002;55:701–14.
Tanaka M, Fernandez-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183–97.
Chari ST, Yadav D, Smyrk TC, DiMagno EP, Miller LJ, Raimondo M, et al. Study of recurrence after surgical resection of intraductal papillary mucinous neoplasm of the pancreas. Gastroenterology. 2002;123:1500–7.
Maire F, Hammel P, Terris B, Paye F, Scoazec JY, Cellier C, et al. Prognosis of malignant intraductal papillary mucinous tumours of the pancreas after surgical resection. Comparison with pancreatic ductal adenocarcinoma. Gut. 2002;51:717–22.
Sohn TA, Yeo CJ, Cameron JL, Hruban RH, Fukushima N, Campbell KA, et al. Intraductal papillary mucinous neoplasms of the pancreas: an updated experience. Ann Surg. 2004;239:788–97.
D’Angelica M, Brennan MF, Suriawinata AA, Klimstra D, Conlon KC. Intraductal papillary mucinous neoplasms of the pancreas: an analysis of clinicopathologic features and outcome. Ann Surg. 2004;239:400–8.
Raut CP, Cleary KR, Staerkel GA, Abbruzzese JL, Wolff RA, Lee JH, et al. Intraductal papillary mucinous neoplasms of the pancreas: effect of invasion and pancreatic margin status on recurrence and survival. Ann Surg Oncol. 2006;13:582–94.
Poultsides GA, Reddy S, Cameron JL, Hruban RH, Pawlik TM, Ahuja N, et al. Histopathologic basis for the favorable survival after resection of intraductal papillary mucinous neoplasm-associated invasive adenocarcinoma of the pancreas. Ann Surg. 2010;251:470–6.
Fernandez-del Castillo C, Adsay NV. Intraductal papillary mucinous neoplasms of the pancreas. Gastroenterology. 2010;139:708–13, e701–2.
Distler M, Kersting S, Niedergethmann M, Aust DE, Franz M, Rückert F, et al. Pathohistological subtype predicts survival in patients with intraductal papillary mucinous neoplasm (IPMN) of the pancreas. Ann Surg. 2013;258:324–30.
Furukawa T, Hatori T, Fujita I, Yamamoto M, Kobayashi M, Ohike N, et al. Prognostic relevance of morphological types of intraductal papillary mucinous neoplasms of the pancreas. Gut. 2011;60:509–16.
Mino-Kenudson M, Fernandez-del Castillo C, Baba Y, Valsangkar NP, Liss AS, Hsu M, et al. Prognosis of invasive intraductal papillary mucinous neoplasm depends on histological and precursor epithelial subtypes. Gut. 2011;60:1712–20.
Adsay NV, Pierson C, Sarkar F, Abrams J, Weaver D, Conlon KC, et al. Colloid (mucinous noncystic) carcinoma of the pancreas. Am J Surg Pathol. 2001;25:26–42.
Society JP. Classification of pancreatic carcinoma. 3rd ed. Tokyo: Kanehara & Co, Ltd; 2011.
Longnecker DS, Adler G, Hruban RH, et al. Serous cystic neoplasms of the pancreas. Tumors of the exocrine pancreas. In: Hamilton SR, Bltonen LA, editors. Pathology and genetics of tumours of the digestive system Lyon: IARC Press; 2000.
Tanaka M, Chari S, Adsay V, Fernandez-del Castillo C, Falconi M, Shimizu M, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006;6:17–32.
Kang MJ, Lee KB, Jang JY, Han IW, Kim SW. Evaluation of clinical meaning of histological subtypes of intraductal papillary mucinous neoplasm of the pancreas. Pancreas. 2013;42:959–66.
Talamini G, Zamboni G, Salvia R, Capelli P, Sartori N, Casetti L, et al. Intraductal papillary mucinous neoplasms and chronic pancreatitis. Pancreatology. 2006;6:626–34.
Adsay NV, Merati K, Basturk O, Iacobuzio-Donahue C, Levi E, Cheng JD, et al. Pathologically and biologically distinct types of epithelium in intraductal papillary mucinous neoplasms: delineation of an “intestinal” pathway of carcinogenesis in the pancreas. Am J Surg Pathol. 2004;28:839–48.
Ban S, Naitoh Y, Mino-Kenudson M, Sakurai T, Kuroda M, Koyama I, et al. Intraductal papillary mucinous neoplasm (IPMN) of the pancreas: its histopathologic difference between 2 major types. Am J Surg Pathol. 2006;30:1561–9.
Nakamura A, Horinouchi M, Goto M, Nagata K, Sakoda K, Takao S, et al. New classification of pancreatic intraductal papillary-mucinous tumour by mucin expression: its relationship with potential for malignancy. J Pathol. 2002;197:201–10.
Hibi Y, Fukushima N, Tsuchida A, Sofuni A, Itoi T, Moriyasu F, et al. Pancreatic juice cytology and subclassification of intraductal papillary mucinous neoplasms of the pancreas. Pancreas. 2007;34:197–204.
Monzen M, Shimizu K, Hatori T, Furukawa T, Shiratori K. Usefulness of cell block cytology for preoperative grading and typing of intraductal papillary mucinous neoplasms. Pancreatology. 2013;13:369–78.
Hisaka T, Horiuchi H, Uchida S, Ishikawa H, Kawahara R, Kawashima Y, et al. Potential usefulness of mucin immunohistochemical staining of preoperative pancreatic biopsy or juice cytology specimens in the determination of treatment strategies for intraductal papillary mucinous neoplasm. Oncol Rep. 2013;30:2035–41.
Hara T, Ikebe D, Odaka A, Sudo K, Nakamura K, Yamamoto H, et al. Preoperative histological subtype classification of intraductal papillary mucinous neoplasms (IPMN) by pancreatic juice cytology with MUC stain. Ann Surg. 2013;257:1103–11.
Ideno N, Ohtsuka T, Kono H, Fujiwara K, Oda Y, Aishima S, et al. Intraductal papillary mucinous neoplasms of the pancreas with distinct pancreatic ductal adenocarcinomas are frequently of gastric subtype. Ann Surg. 2013;258:141–51.
Disclosure
Suguru Yamada, Tsutomu Fujii, Tsutomu Fujii, Mitsuro Kanda, Goro Nakayama, Hiroyuki Sugimoto, Masahiko Koike, Shuji Nomoto, Michitaka Fujiwara, Akimasa Nakao, and Yasuhiro Kodera have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yamada, S., Fujii, T., Shimoyama, Y. et al. Clinical Implication of Morphological Subtypes in Management of Intraductal Papillary Mucinous Neoplasm. Ann Surg Oncol 21, 2444–2452 (2014). https://doi.org/10.1245/s10434-014-3565-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-3565-1