Abstract
Background
The circumferential resection margin (CRM) is a strong prognostic factor in rectal cancer. The purpose of this study was to investigate the relationship between CRM distance and recurrence in patients with locally advanced rectal cancer who received preoperative chemoradiotherapy (CRT).
Methods
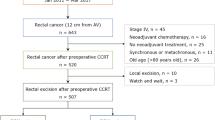
We analyzed data for 561 patients who underwent preoperative CRT and curative surgery for locally advanced rectal cancer between August 2001 and December 2008. CRM was divided into four groups: group 1, CRM > 2 mm; group 2, 1.1–2.0 mm; group 3, 0.1–1.0 mm; and group 4, 0 mm. We assessed the associations of CRM with local recurrence and disease-free survival.
Results
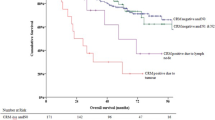
Groups 1, 2, 3, and 4 comprised 487, 36, 20, and 18 patients, respectively. The local recurrence rate was highest and the disease-free survival rate was lowest in group 4, followed by groups 3, 2, and 1. Survival was similar between groups 2 and 1. Local recurrence rates were lower in groups 3, 2, and 1 than in group 4 [hazard ratio (HR) 0.28, 95 % confidence interval (CI) 0.09–0.91, P = 0.035; HR 0.11, 95 % CI 0.03–0.46, P = 0.002; HR 0.18, 95 % CI 0.08–0.42, P < 0.0001, respectively]. Disease-free survival rates were higher in groups 3, 2, and 1 than in group 4 (HR 0.32, 95 % CI 0.13–0.75, P = 0.009; HR 0.24, 95 % CI 0.10–0.54, P = 0.001; HR 0.26, 95 % CI 0.14–0.48, P < 0.0001, respectively).
Conclusions
After preoperative CRT, CRM distance provides useful information for risk stratification in the recurrence of rectal cancer.

Similar content being viewed by others
References
Quirke P, Durdey P, Dixon MF, Williams NS. Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumour spread and surgical excision. Lancet. 1986;2:996–99.
Birbeck KF, Macklin CP, Tiffin NJ, et al. Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann Surg. 2002;235:449–57.
Wibe A, Rendedal PR, Svensson E, et al. Prognostic significance of the circumferential resection margin following total mesorectal excision for rectal cancer. Br J Surg. 2002;89:327–34.
Rullier E, Goffre B, Bonnel C, Zerbib F, Caudry M, Saric J. Preoperative radiochemotherapy and sphincter-saving resection for T3 carcinomas of the lower third of the rectum. Ann Surg. 2001;234:633–40.
den Dulk M, Collette L, van de Velde CJ, et al. Quality of surgery in T3-4 rectal cancer: involvement of circumferential resection margin not influenced by preoperative treatment. Results from EORTC trial 22921. Eur J Cancer. 2007;43:1821–8.
Nagtegaal ID, Quirke P. What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol. 2008;26:303–12.
Gosens MJ, Klaassen RA, Tan-Go I, et al. Circumferential margin involvement is the crucial prognostic factor after multimodality treatment in patients with locally advanced rectal carcinoma. Clin Cancer Res. 2007;13:6617–23.
Adam IJ, Mohamdee MO, Martin IG, et al. Role of circumferential margin involvement in the local recurrence of rectal cancer. Lancet. 1994;344:707–11.
Nagtegaal ID, Marijnen CA, Kranenbarg EK, van de Velde CJ, van Krieken JH. Circumferential margin involvement is still an important predictor of local recurrence in rectal carcinoma: not one millimeter but two millimeters is the limit. Am J Surg Pathol. 2002;26:350–7.
Glynne-Jones R, Mawdsley S, Novell JR. The clinical significance of the circumferential resection margin following preoperative pelvic chemo-radiotherapy in rectal cancer: why we need a common language. Colorectal Dis. 2006;8:800–7.
de Haas-Kock DF, Baeten CG, Jager JJ, et al. Prognostic significance of radial margins of clearance in rectal cancer. Br J Surg. 1996;83:781–5.
Tilney HS, Rasheed S, Northover JM, Tekkis PP. The influence of circumferential resection margins on long-term outcomes following rectal cancer surgery. Dis Colon Rectum. 2009;52:1723–9.
Luna-Perez P, Bustos-Cholico E, Alvarado I, et al. Prognostic significance of circumferential margin involvement in rectal adenocarcinoma treated with preoperative chemoradiotherapy and low anterior resection. J Surg Oncol. 2005;90:20–5.
Wittekind C, Compton C, Quirke P, et al. A uniform residual tumor (R) classification: integration of the R classification and the circumferential margin status. Cancer. 2009;115:3483–8.
Dent OF, Haboubi N, Chapuis PH, et al. Assessing the evidence for an association between circumferential tumour clearance and local recurrence after resection of rectal cancer. Colorectal Dis. 2007;9:112–21.
Hwang MR, Park JW, Kim DY, et al. Prognostic impact of peritonealisation in rectal cancer treated with preoperative chemoradiotherapy: extraperitoneal versus intraperitoneal rectal cancer. Radiother Oncol. 2010;94:353–8.
Kim DY, Jung KH, Kim TH, et al. Comparison of 5-fluorouracil/leucovorin and capecitabine in preoperative chemoradiotherapy for locally advanced rectal cancer. Int J Radiat Oncol Biol Phys. 2007;67:378–84.
Quirke P, Dixon MF. The prediction of local recurrence in rectal adenocarcinoma by histopathological examination. Int J Colorectal Dis. 1988;3:127–31.
Greene FL, Page DL, Fleming ID, et al. American Joint Committee on Cancer staging manual. 6th ed. New York: Springer; 2002.
Hamilton SR, Vogelstein B, Kudo S, et al. Carcinoma of the colon and rectum. In: Hamilton SR, Aaltonen LA editors. World Health Organization classification of tumours. Pathology and genetics of tumours of the digestive system. Lyon: IARC Press, Lyon; 2000. p. 104–19.
Dworak O, Keilholz L, Hoffmann A. Pathological features of rectal cancer after preoperative radiochemotherapy. Int J Colorectal Dis. 1997;12:19–23.
Marijnen CA, Nagtegaal ID, Kapiteijn E, et al. Radiotherapy does not compensate for positive resection margins in rectal cancer patients: report of a multicenter randomized trial. Int J Radiat Oncol Biol Phys. 2003;55:1311–20.
Mawdsley S, Glynne-Jones R, Grainger J, et al. Can histopathologic assessment of circumferential margin after preoperative pelvic chemoradiotherapy for T3-T4 rectal cancer predict for 3-year disease-free survival? Int J Radiat Oncol Biol Phys. 2005;63:745–52.
Marijnen CA, Nagtegaal ID, Klein Kranenbarg E, et al. No downstaging after short-term preoperative radiotherapy in rectal cancer patients. J Clin Oncol. 2001;19:1976–84.
Sebag-Montefiore D, Stephens RJ, Steele R, et al. Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial. Lancet. 2009;373:811–20.
Bujko K, Nowacki MP, Nasierowska-Guttmejer A, et al. Sphincter preservation following preoperative radiotherapy for rectal cancer: report of a randomised trial comparing short-term radiotherapy vs. conventionally fractionated radiochemotherapy. Radiother Oncol. 2004;72:15–24.
Bosset JF, Calais G, Mineur L, et al. Enhanced tumorocidal effect of chemotherapy with preoperative radiotherapy for rectal cancer: preliminary results—EORTC 22921. J Clin Oncol. 2005;23:5620–7.
Wheeler JM, Dodds E, Warren BF, et al. Preoperative chemoradiotherapy and total mesorectal excision surgery for locally advanced rectal cancer: correlation with rectal cancer regression grade. Dis Colon Rectum. 2004;47:2025–31.
Rullier A, Laurent C, Vendrely V, Le Bail B, Bioulac-Sage P, Rullier E. Impact of colloid response on survival after preoperative radiotherapy in locally advanced rectal carcinoma. Am J Surg Pathol. 2005;29:602–6.
Acknowledgment
This study was supported by a grant from the National Cancer Center of Korea (NCC-0910160) and by the Converging Research Center Program funded by the Ministry of Education, Science and Technology (project 1131150).
Conflict of interest
The authors indicated no potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hwang, M.R., Park, J.W., Park, S. et al. Prognostic Impact of Circumferential Resection Margin in Rectal Cancer Treated with Preoperative Chemoradiotherapy. Ann Surg Oncol 21, 1345–1351 (2014). https://doi.org/10.1245/s10434-014-3484-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-3484-1