Abstract
Background
The purposes of this study were to clarify the risk factors for supraclavicular lymph node (SCLN) metastasis and the survival benefit from cervical lymph node (LN) dissections in patients with clinically submucosal (cT1b) carcinoma of the thoracic esophagus.
Methods
A total of 86 patients with this disease who underwent esophagectomy with 3-field lymph node dissection were retrospectively reviewed. Multivariate logistic regression and Cox proportional hazard model were used to identify the independent risk factors for SCLN metastasis and prognostic factors, respectively. An index calculated by multiplying the frequency of metastasis at nodal basin and the 5-year overall survival rate of patients with metastasis at that basin were used to assess the therapeutic outcomes.
Results
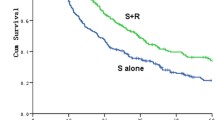
A total of 40 patients (47 %) were found to have pathological LN metastasis. Also, 13 patients (15 %) had cervical LN metastasis: 6 and 7 with carcinoma of the upper and mid-thoracic esophagus, respectively. SCLN metastasis was found in 6 patients (7 %); however, there was no independent risk factor for SCLN metastasis. The 5-year overall survival rate was 72.5 %. Cervical LN metastasis was an independent prognostic factor (p = .04; odds ratio 2.55; 95 % confidence interval 1.03–6.31); however, there was no significant difference in survival between patients with SCLN metastasis and those without (p = .06). The calculated index of estimated benefit from cervical LN dissections was 6.9, following upper mediastinal LN of 15.6 and perigastric LN of 8.3.
Conclusions
We could not identify risk factors to predict SCLN metastasis. Cervical LN dissection should not be omitted in patients with cT1b carcinoma, especially of the upper and mid-thoracic esophagus.

Similar content being viewed by others
References
Enzinger PC, Mayer RJ. Esophageal cancer. N Engl J Med. 2003;349:2241–52.
Pennathur A, Gibson MK, Jobe BA, Luketich JD. Oesophageal carcinoma. Lancet. 2013;381:400–12.
Nishimaki T, Suzuki T, Kanda T, Obinata I, Komukai S, Hatakeyama K. Extended radical esophagectomy for superficially invasive carcinoma of the esophagus. Surgery. 1999;125:142–7.
Igaki H, Kato H, Tachimori Y, Daiko H, Fukaya M, Yajima S, Nakanishi Y. Clinicopathologic characteristics and survival of patients with clinical Stage I squamous cell carcinomas of the thoracic esophagus treated with three-field lymph node dissection. Eur J Cardiothorac Surg. 2001;20:1089–94.
Grotenhuis BA, van Heijl M, Zehetner J, Moons J, Wijnhoven BP, van Berge Henegouwen MI, et al. Surgical management of submucosal esophageal cancer: extended or regional lymphadenectomy? Ann Surg. 2010;252:823–30.
Sobin LH, Gospodarowicz MK, Wittekind Ch, editors. TNM classification of malignant tumours, 7th ed. Hoboken: Wiley-Blackwell, 2009.
Nishimaki T, Suzuki T, Suzuki S, Kuwabara S, Hatakeyama K. Outcomes of extended radical esophagectomy for thoracic esophageal cancer. J Am Coll Surg. 1998;186:306–12.
Japan Esophageal Society. Japanese classification of esophageal cancer, 10th ed. Tokyo: Kanehara, 2008.
Yamashita H, Katai H, Morita S, Saka M, Taniguchi H, Fukagawa T. Optimal extent of lymph node dissection for Siewert type II esophagogastric junction carcinoma. Ann Surg. 2011;254:274–80.
Tabira Y, Yasunaga M, Tanaka M, Nakano K, Sakaguchi T, Nagamoto N, et al. Recurrent nerve nodal involvement is associated with cervical nodal metastasis in thoracic esophageal carcinoma. J Am Coll Surg. 2000;191:232–7.
Li B, Chen H, Xiang J, Zhang Y, Li C, Hu H, et al. Pattern of lymphatic spread in thoracic esophageal squamous cell carcinoma: A single-institution experience. J Thorac Cardiovasc Surg. 2012;144:778–85.
Kuge K, Murakami G, Mizobuchi S, Hata Y, Aikou T, Sasaguri S. Submucosal territory of the direct lymphatic drainage system to the thoracic duct in the human esophagus. J Thorac Cardiovasc Surg. 2003;125:1343–9.
Mizutani M, Murakami G, Nawata S, Hitrai I, Kimura Y. Anatomy of right recurrent nerve node: why does early metastasis of esophageal cancer occur in it? Surg Radiol Anat. 2006;28:333–8.
Tachimori Y, Nagai Y, Kanamori N, Hokamura N, Igaki H. Pattern of lymph node metastases of esophageal squamous cell carcinoma based on the anatomical lymphatic drainage system. Dis Esophagus. 2011;24:33–8.
Nathanson SD. Insights into the mechanisms of lymph node metastasis. Cancer. 2003;98:413–23.
Nakagawa S, Nishimaki T, Kosugi S, Ohashi M, Kanda T, Hatakeyama K. Cervical lymphadenectomy is beneficial for patients with carcinoma of the upper and mid-thoracic esophagus. Dis Esophagus. 2003;16:4–8.
Lerut T, Nafteux P, Moons J, Coosemans W, Decker G, De Leyn P, et al. Three-field lymphadenectomy for carcinoma of the esophagus and gastroesophageal junction in 174 R0 resections: impact on staging, disease-free survival, and outcome: a plea for adaptation of TNM classification in upper-half esophageal carcinoma. Ann Surg. 2004;240:962–72.
Shimada H, Okazumi S, Matsubara H, Nabeya Y, Shiratori T, Shimizu T, et al. Impact of the number and extent of positive lymph nodes in 200 patients with thoracic esophageal squamous cell carcinoma after three-field lymph node dissection. World J Surg. 2006;30:1441–9.
The Registration Committee for Esophageal Cancer. Comprehensive registry of esophageal cancer in Japan, 2004. Chiba: The Japan Esophageal Society, 2012.
Disclosures
No commercial interest and financial or material support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kosugi, Si., Kawaguchi, Y., Kanda, T. et al. Cervical Lymph Node Dissection for Clinically Submucosal Carcinoma of the Thoracic Esophagus. Ann Surg Oncol 20, 4016–4021 (2013). https://doi.org/10.1245/s10434-013-3141-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-013-3141-0