Abstract
Background
Current National Comprehensive Cancer Network guidelines recommend repeat imaging 6–12 months after a benign radiologic–pathologic concordant image-guided breast biopsy. We hypothesized that interval imaging <12 months after benign concordant biopsy has a low cancer yield and increases health care costs.
Methods
An institutional review board-approved retrospective chart review identified 689 patients who underwent image-guided breast biopsy at Bryn Mawr Hospital between January and December 2010. Charts were evaluated for documentation of radiologic–pathologic concordance.
Results
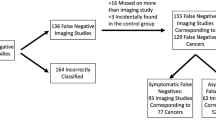
Of 689 patients, 188 (27 %) had malignant pathology, 3 (0.4 %) had nonbreast pathology, and 498 (72.3 %) had benign pathology. Of 498 patients with benign findings, 44 (8.8 %) underwent surgical excision as a result of discordance, atypia, papillary lesion, or other benign finding. Of the remaining 454 patients who did not undergo excision, 337 (74.2 %) had documented radiologic–pathologic concordance. Interval imaging <12 months after benign biopsy was obtained in 182 (54.0 %) concordant patients. Five (2.7 %) patients had suspicious [American College of Radiology Breast Imaging-Reporting and Data System (BI-RADS) 4] findings on follow-up imaging. Only one breast cancer was identified, representing 0.5 % (95 % confidence interval 0–3.4) of all benign concordant patients undergoing interval imaging. The cost of detecting a missed cancer with interval imaging after benign concordant biopsy was $41,813.77 in this cohort.
Conclusions
Interval imaging performed <12 months after benign concordant breast biopsy demonstrated a low yield for the detection of breast cancer and resulted in increased health care costs. Our data support the policy for discontinuation of routine interval imaging after benign concordant biopsy.


Similar content being viewed by others
References
Silverstein MJ, Recht A, Lagios MD, et al. Image-detected breast cancer: state of the art diagnosis and treatment. International Breast Cancer Consensus Conference III. J Am Coll Surg. 2009;209:504–20.
Verkooijen HM. Diagnostic accuracy of stereotactic large-core needle biopsy for nonpalpable breast disease: results of a multicenter prospective study with 95 % surgical confirmation. Int J Cancer. 2002;99:853–9.
Pijnappel RM, van den Donk M, Holland R, et al. Diagnostic accuracy for different strategies of image-guided breast intervention in cases of nonpalpable breast lesions. Br J Cancer. 2004;90:595–600.
National Comprehensive Cancer Network. NCCN guidelines, version 1: breast cancer screening and diagnosis. 2012. http://www.nccn.org. Accessed 10 Sept 2012.
Shin S, Schneider HB, Cole FJ, et al. Follow-up recommendations for benign breast biopsies. Breast J. 2006;12:413–7.
Lee CH, Philpotts LE, Horvath LJ, et al. Follow-up of breast lesions diagnosed as benign with stereotactic core-needle biopsy: frequency of mammographic change and false-negative rate. Radiology. 1999;212:189–94.
Liberman L, Drotman M, Morris EA, et al. Imaging-histologic discordance at percutaneous breast biopsy: an indicator of missed cancer. Cancer. 2000;89:2538–46.
American College of Radiology. Breast Imaging Reporting and Data System (BI-RADS) breast imaging atlas. 4th ed. Reston: American College of Radiology; 2003.
ASPE Technical Expert Panel on Improving Cancer Policy Research through Information Technology. The importance of radiology and pathology in the diagnosis and staging of cancer: mammography as a case study. 2010. http://aspe.hhs.gov/sp/reports/2010/PathRad/index.shtml. Accessed 3 April 2013.
Sickles EA. Periodic mammographic follow-up of probably benign lesions: results in 3,184 consecutive cases. Radiology. 1991;179:463–8.
Jackman RJ, Nowels KW, Rodriguez-Soto J, et al. Stereotactic, automated, large-core needle biopsy of nonpalpable breast lesions: false-negative and histologic underestimation rates after long-term follow-up. Radiology. 1999;210:799–805.
Margolin FR, Leung JW, Jacobs RP, et al. Percutaneous imaging-guided core breast biopsy: 5 years’ experience in a community hospital. AJR Am J Roentgenol. 2001;177:559–64.
Lee JM, Kaplan JB, Murray MP, et al. Imaging-histologic discordance at MRI-Guided 9-gauge vacuum-assisted breast biopsy. AJR Am J Roentgenol. 2007;189:852–9.
American Society of Breast Surgeons. Position statement of concordance assessment of image-guided breast biopsies and management of borderline or high-risk lesions. 2011. http://www.breastsurgeons.org/statement/index.php. Accessed 3 April 2013.
Chubak J, Boudreau DM, Fishman PA, et al. Cost of breast-related care in the year following false positive screening mammograms. Med Care. 2010;48:815–20.
Disclosure
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Manjoros, D.T., Collett, A.E., Alberty-Oller, J.J. et al. The Value of 6-Month Interval Imaging after Benign Radiologic–Pathologic Concordant Minimally Invasive Breast Biopsy. Ann Surg Oncol 20, 3163–3168 (2013). https://doi.org/10.1245/s10434-013-3114-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-013-3114-3