Abstract
Background
Criteria for resectability of colon cancer liver metastases (CLM) are evolving, yet little is known about how physicians choose a therapeutic strategy for potentially resectable CLM.
Methods
Physicians completed a national Web-based survey that consisted of varied CLM conjoint tasks. Respondents chose among three treatment strategies: immediate liver resection (LR), preoperative chemotherapy followed by surgery (C → LR), or palliative chemotherapy (PC). Data were analyzed by multinomial logistic regression, yielding odds ratios (OR).
Results
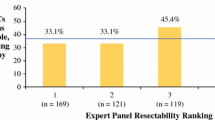
Of 219 respondents, 79 % practiced at academic centers and 63 % were in practice ≥10 years. Median number of cases evaluated was four per month. Surgical training varied: 51 % surgical oncology, 44 % hepato-pancreato-biliary/transplantation, 5 % no fellowship. Although each factor affected the choice of CLM therapy, the relative effect differed. Hilar lymph node disease predicted a strong aversion to LR with surgeons more likely to choose C → LR (OR 8.92) or PC (OR 49.9). Solitary lung metastasis also deterred choice of LR, with respondents favoring C → LR (OR 4.43) or PC (OR 6.97). After controlling for clinical factors, surgeons with more years in practice were more likely to choose PC over C → LR (OR 1.94) (P = 0.005). Surgical oncology-trained surgeons were more likely than hepatobiliary/transplant-trained surgeons to choose C → LR (OR 2.53) or PC (OR 4.15) (P < 0.001).
Conclusions
This is the first nationwide study to define the relative impact of key clinical factors on choice of therapy for CLM. Although clinical factors influence choice of therapy, surgical subspeciality and physician experience are also important determinants of care.

Similar content being viewed by others
References
Pawlik TM, Choti MA. Surgical therapy for colorectal metastases to the liver. J Gastrointest Surg. 2007;11:1057–77.
Pawlik TM, Choti MA. Shifting from clinical to biologic indicators of prognosis after resection of hepatic colorectal metastases. Curr Oncol Rep. 2007;9:193–201.
Pawlik TM, Vauthey JN. Surgical margins during hepatic surgery for colorectal liver metastases: complete resection not millimeters defines outcome. Ann Surg Oncol. 2008;15:677–9.
Al-Sahaf O, Al-Azawi D, Al-Khudairy A, et al. Referral patterns of patients with liver metastases due to colorectal cancer for resection. Int J Colorectal Dis. 2009;24:79–82.
Fong Y, Fortner J, Sun RL, et al. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230:309–18.
Nordlinger B, Guiguet M, Vaillant JC, et al. Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer. 1996;77:1254–62.
Scheele J, Stangl R, Altendorf-Hofmann A. Hepatic metastases from colorectal carcinoma: impact of surgical resection on the natural history. Br J Surg. 1990;77:1241–6.
de Jong MC, Pulitano C, Ribero D, et al. Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Ann Surg. 2009;250:440–8.
Langenhoff BS, Krabbe PF, Ruers TJ. Computer-based decision making in medicine: a model for surgery of colorectal liver metastases. Eur J Surg Oncol. 2007;33(Suppl 2):S111–7.
Kee F, McDonald P, Kirwan JR, et al. The stated and tacit impact of demographic and lifestyle factors on prioritization decisions for cardiac surgery. QJM. 1997;90:117–23.
Kirwan JR, Currey HL, Brooks PM. Measuring physicians’ judgment—the use of clinical data by Australian rheumatologists. Aus N Z J Med. 1985;15:738–44.
Bridges JF. Stated preference methods in health care evaluation: an emerging methodological paradigm in health economics. Appl Health Econ Health Policy. 2003;2:213–24.
Nathan H, Bridges JF, Schulick RD, et al. Understanding surgical decision making in early hepatocellular carcinoma. J Clin Oncol. 2011;29:619–25.
Hedayat A, Sloane N, Stufken J. Orthogonal arrays: theory and application. New York: Springer; 1999.
Kucirka LM, Namuyinga R, Hanrahan C, et al. Formal policies and special informed consent are associated with higher provider utilization of CDC high-risk donor organs. Am J Transplant. 2009;9:629–35.
Timmermans DR, Gooszen AW, Geelkerken RH, et al. Analysis of the variety in surgeons’ decision strategies for the management of left colonic emergencies. Med Care. 1997;35:701–13.
Kirwan JR, Chaput de Saintonge DM, Joyce CR, et al. Inability of rheumatologists to describe their true policies for assessing rheumatoid arthritis. Ann Rheum Dis. 1986;45:156–61.
Heatherton TF, Mahamedi F, Striepe M, et al. A 10-year longitudinal study of body weight, dieting, and eating disorder symptoms. J Abnorm Psychology. 1997;106:117–25.
Viney R, Lancsar E, Louviere J. Discrete choice experiments to measure consumer preferences for health and healthcare. Expert Rev Pharmacoeconom Outcomes Res. 2002;2:319–26.
Phillips KA, Maddala T, Johnson FR. Measuring preferences for health care interventions using conjoint analysis: an application to HIV testing. Health Serv Res. 2002;37:1681–705.
Ijzerman MJ, van Til JA, Snoek GJ. Comparison of two multi-criteria decision techniques for eliciting treatment preferences in people with neurological disorders. Patient. 2008;1:265–72.
Yedibela S, Klein P, Feuchter K, et al. Surgical management of pulmonary metastases from colorectal cancer in 153 patients. Ann Surg Oncol. 2006;13:1538–44.
Girard P, Ducreux M, Baldeyrou P, et al. Surgery for lung metastases from colorectal cancer: analysis of prognostic factors. J Clin Oncol. 1996;14:2047–53.
Iizasa T, Suzuki M, Yoshida S, et al. Prediction of prognosis and surgical indications for pulmonary metastasectomy from colorectal cancer. Ann Thorac Surg. 2006;82:254–60.
Pulitano C, Bodingbauer M, Aldrighetti L, et al. Liver resection for colorectal metastases in presence of extrahepatic disease: results from an international multi-institutional analysis. Ann Surg Oncol. 2011;18:1380–8.
Elias D, Liberale G, Vernerey D, et al. Hepatic and extrahepatic colorectal metastases: when resectable, their localization does not matter, but their total number has a prognostic effect. Ann Surg Oncol. 2005;12:900–9.
Frances CD, Shlipak MG, Noguchi H, et al. Does physician specialty affect the survival of elderly patients with myocardial infarction? Health Serv Res. 2000;35:1093–116.
Parekh V, Saint S, Furney S, et al. What effect does inpatient physician specialty and experience have on clinical outcomes and resource utilization on a general medical service? J Gen Intern Med. 2004;19:395–401.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nathan, H., Bridges, J.F., Cosgrove, D.P. et al. Treating Patients with Colon Cancer Liver Metastasis: A Nationwide Analysis of Therapeutic Decision Making. Ann Surg Oncol 19, 3668–3676 (2012). https://doi.org/10.1245/s10434-012-2564-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-012-2564-3